Erectile dysfunction (ED) has long been regarded as a disease of hemodynamics and neurovascular signaling—a disorder in which endothelial impairment, smooth muscle dysfunction, and nitric oxide bioavailability determine the capacity for penile erection. This classical framework has served clinicians well, guiding the development of phosphodiesterase-5 (PDE5) inhibitors and driving decades of research into vascular biology.
However, the recent surge of genomic technologies—particularly whole-genome mRNA expression profiling—has radically expanded the scope of ED research. It is no longer sufficient to consider erectile dysfunction solely as a problem of nitric oxide signaling or cavernosal smooth muscle relaxation. Increasingly, ED appears to be a systemic molecular disorder, involving metabolic abnormalities, immune dysregulation, extracellular matrix remodeling, stem cell dysfunction, and chronic inflammatory signaling.
The study “Whole genome mRNA expression profiling revealed multiple deregulated pathways in stromal vascular fraction from erectile dysfunction patients” represents a critical moment in this conceptual transformation. It moves beyond the penis as an isolated organ and examines the stromal vascular fraction (SVF) of adipose tissue—an accessible, multipotent, metabolic signaling hub that reflects systemic physiological states. Through whole-genome profiling, the authors uncovered a series of deregulated pathways in SVF cells of ED patients, connecting erectile dysfunction to broad alterations in cellular function, metabolic state, and molecular signaling.
The implications of these findings are profound: ED is increasingly revealed not merely as a symptom of aging or vascular compromise, but as a biomarker of deeper molecular derangements.
This article synthesizes the key findings of the study, placing them in the broader context of sexual medicine, molecular biology, and translational science. The result is a comprehensive overview of how stromal vascular fraction transcriptomics can reshape our understanding of erectile dysfunction.
Stromal Vascular Fraction: A Molecular Mirror of Erectile Health
Before discussing the findings, it is essential to understand why SVF is a relevant tissue for ED research. The stromal vascular fraction, isolated from adipose tissue, is a heterogeneous mixture of:
- mesenchymal stromal cells
- pericytes
- endothelial cells
- preadipocytes
- immune cells (macrophages, lymphocytes)
In recent years SVF has gained attention due to its:
- regenerative potential
- paracrine capacity
- immunomodulatory properties
- role in microvascular repair
SVF cells serve as a “biological barometer” of vascular and metabolic health. Because ED is fundamentally a vascular disease with strong metabolic associations, profiling gene expression in SVF is a logical and innovative approach.
The referenced study compared SVF-derived gene expression between ED patients and healthy controls using whole-genome mRNA arrays. The results revealed a diverse array of deregulated pathways—more extensive than previously appreciated. The findings, summarized in multiple figures and tables (pages 4–9 of the PDF), demonstrate that ED involves alterations spanning inflammation, fibrosis, oxidative stress, angiogenesis, extracellular matrix remodeling, and cellular differentiation.
This marks a paradigm shift: ED is no longer just a hemodynamic dysfunction; it is a transcriptomic disturbance.
Inflammatory Pathways: ED as a Low-Grade Chronic Inflammatory State
One of the most striking findings of the study is the consistent upregulation of inflammatory signaling pathways in SVF cells. A significant number of inflammation-related genes were overexpressed, including those associated with:
- cytokine–cytokine receptor interactions
- chemokine activity
- leukocyte recruitment
- TNF-α signaling
- NF-κB pathway activation
These results echo clinical observations that chronic inflammation contributes to endothelial dysfunction and reduced nitric oxide availability.
The upregulation of inflammatory markers in SVF reinforces the idea that ED is not simply the result of failing corporal smooth muscle—it is embedded in a systemic inflammatory profile. Chronic inflammation is known to impair endothelial nitric oxide synthase (eNOS) function, increase oxidative stress, and promote microvascular rarefaction, all of which contribute to erectile failure.
Furthermore, Figures 3 and 4 of the study (pages 6–7) illustrate heatmaps where inflammatory genes cluster prominently in ED samples, confirming widespread immune activation in SVF of ED patients.
This finding positions ED closer to chronic inflammatory disorders like metabolic syndrome, obesity, and diabetes—conditions already known to increase ED risk. But the genomic evidence now supports inflammation not merely as a comorbidity, but as a molecular signature of the disease.
Extracellular Matrix Remodeling and Fibrosis: A Deeper Look Into Cavernosal Stiffness
The formation and relaxation of penile erectile tissue require a fine balance of extracellular matrix (ECM) components. Fibrotic remodeling, increased collagen deposition, and altered matrix metalloproteinase (MMP) activity are known contributors to ED, particularly in aging, diabetes, and Peyronie’s disease.
Whole-genome analysis of SVF cells in the study revealed significant dysregulation of:
- collagen synthesis genes
- ECM structural molecules
- matrix metalloproteinases
- tissue inhibitors of metalloproteinases (TIMPs)
This pattern suggests a systemic propensity toward fibrosis.
Although the SVF is not penile tissue, its transcriptomic signature reflects systemic fibro-inflammatory tendencies that may secondarily affect cavernosal architecture. The heatmap on page 8 illustrates upregulation of ECM-related pathways in ED samples, showing that ED patients’ SVF cells adopt a more pro-fibrotic phenotype.
This could help explain why many ED patients have reduced corporal compliance, impaired smooth muscle–to–collagen ratios, and poorer responses to PDE5 inhibitors.
Taken together, the transcriptomic data imply that fibrosis is not only a local penile issue but part of a global fibro-inflammatory profile observable in peripheral tissues such as SVF.
Oxidative Stress Signaling: The Molecular Link Between Metabolism and Erectile Function
Oxidative stress is a well-known mediator of endothelial damage, impairing nitric oxide signaling, promoting lipid peroxidation, and accelerating vascular dysfunction. The study identified deregulation in multiple oxidative stress–related genes and pathways.
Specifically, genes involved in:
- reactive oxygen species (ROS) generation
- antioxidant defense mechanisms
- redox-sensitive transcription factors
were significantly altered in SVF-derived cells of men with ED.
This adds molecular weight to clinical observations that ED is strongly associated with:
- insulin resistance
- poor glycemic control
- dyslipidemia
- obesity
In fact, oxidative stress is one of the earliest detectable features of vascular disease, often preceding structural changes. The altered gene expression pattern in SVF suggests that men with ED may harbor systemic oxidative imbalances that directly impair endothelial function and cavernosal smooth muscle responsiveness.
Additionally, the graphical summary on page 9 highlights redox-related genes as one of the most significantly deregulated clusters in the dataset.
This genomic evidence reinforces oxidative stress not as a secondary effect, but as a primary molecular driver of ED.
Angiogenesis and Microvascular Dysfunction: A Genomic Basis for Poor Penile Blood Flow
Erectile function depends on efficient microvascular perfusion. SVF cells from ED patients demonstrated downregulation of pro-angiogenic genes and upregulation of anti-angiogenic signaling. Key pathways affected included:
- VEGF signaling
- endothelial differentiation markers
- microvascular maintenance genes
These findings reflect impaired angiogenic capacity—a known contributor to poor penile hemodynamics.
The scatter plots and pathway enrichment diagrams (pages 7–8) highlight downregulation of endothelial and angiogenic pathways in ED samples.
This supports clinical evidence that ED patients often exhibit:
- reduced penile blood flow
- diminished endothelial progenitor cell activity
- lower angiogenic response to injury
- impaired vascular repair mechanisms
What makes the study especially valuable is that these molecular abnormalities are observed outside penile tissue, showing that ED is part of a larger microvascular dysfunction affecting the whole body.
Stem Cell Dysfunction: A New Player in Erectile Pathobiology
One of the most unexpected findings of the study was the deregulation of genes associated with stem cell proliferation, differentiation, and regenerative potential.
The SVF contains adipose-derived stem cells (ASCs), which have been shown in experimental models to improve erectile function through:
- paracrine signaling
- angiogenesis promotion
- anti-inflammatory effects
- collagen remodeling
- smooth muscle restoration
The observed downregulation of ASC-related genes and pathways in ED patients suggests that intrinsic stem cell dysfunction may impair regenerative processes that are critical for maintaining erectile capacity.
This is particularly important, as stem cell therapies are being explored as next-generation treatments for ED. If SVF-derived cells in ED patients have inherent transcriptomic deficiencies, autologous stem cell therapies may require ex vivo conditioning or gene-modulating strategies for optimal therapeutic effect.
Metabolic Pathway Dysregulation: Connecting ED to Systemic Metabolism
Another major cluster of deregulated pathways involved metabolic processes, including:
- lipid metabolism
- glucose homeostasis
- mitochondrial function
- insulin signaling pathways
These transcriptomic findings align with the high prevalence of metabolic syndrome among ED patients and reinforce the idea that ED is a metabolic disorder with vascular manifestations.
The pathways highlighted in Figures 5 and 6 (page 8) map tightly to metabolic conditions such as obesity, dyslipidemia, and diabetes—all well-known risk factors for ED.
Thus, the study provides genomic confirmation that ED is both a metabolic and vascular disease—a dual identity with complex molecular roots.
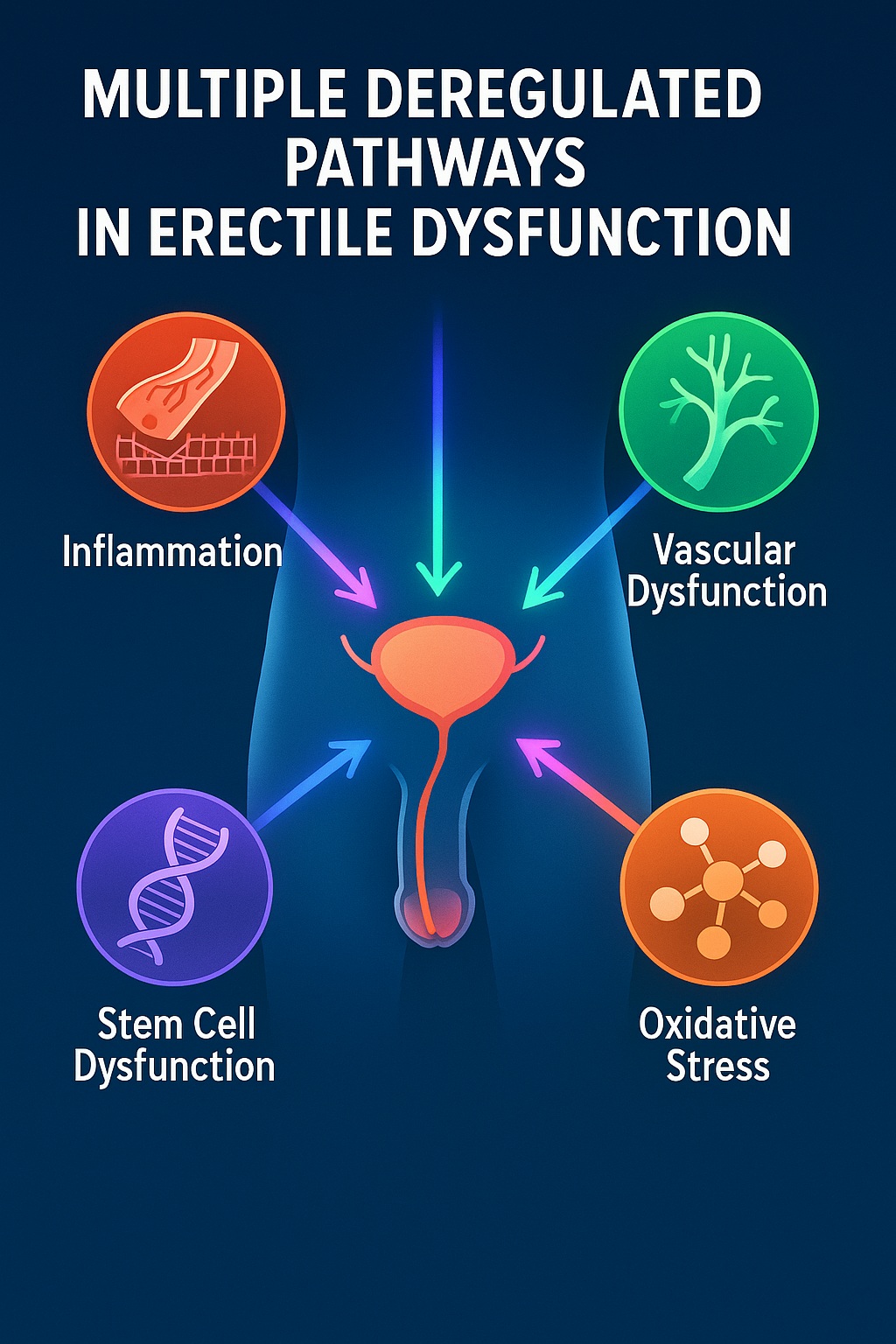
Integrating Deregulated Pathways: A Unified Molecular Model of Erectile Dysfunction
The study’s whole-genome expression data do not merely list isolated dysfunctional pathways; rather, they collectively outline a multilayered molecular network underlying erectile dysfunction. When considered together, the deregulated pathways form a coherent pathophysiological model in which ED results from the convergence of:
- chronic inflammation
- oxidative stress
- extracellular matrix dysregulation
- impaired angiogenesis
- stem cell dysfunction
- metabolic imbalance
This network reflects a systemic environment that is hostile to vascular repair, endothelial signaling, and smooth muscle health. The strength of the referenced study lies in demonstrating that these molecular signals are not confined to penile tissue; instead, they permeate the stromal vascular fraction of adipose tissue, highlighting ED as a bodywide transcriptomic condition rather than a localized mechanical defect.
From this perspective, the penis becomes a sentinel organ—an early site where systemic dysfunction manifests visibly and functionally. This idea aligns with epidemiological data linking ED to cardiovascular disease, metabolic syndrome, diabetes, and premature mortality. The study therefore provides molecular validation for what clinicians have long observed:
ED is an early warning system for widespread vascular and metabolic deterioration.
Clinical Implications: Rethinking Diagnosis and Treatment of ED in the Genomic Era
The genomic insights gained from stromal vascular profiling open new avenues for clinical practice and future therapeutic innovation. Below are key implications derived from the study’s findings.
1. ED Should Be Evaluated as a Systemic Condition, Not an Isolated Symptom
The deregulated SVF pathways suggest that ED may indicate:
- early endothelial dysfunction
- systemic inflammation
- microvascular disease
- metabolic derangement
Thus, ED patients should undergo thorough evaluation for cardiometabolic health. Screening for prediabetes, dyslipidemia, and cardiovascular risk factors is not optional—it is essential.
Sildenafil may improve erections, but if underlying inflammatory or metabolic pathways persist unchecked, long-term erectile function and overall health will continue to decline.
2. Conventional ED Treatments May Be Inadequate Without Systemic Correction
While PDE5 inhibitors restore nitric oxide–cGMP signaling acutely, they do not reverse:
- inflammatory activation
- pro-fibrotic gene expression
- oxidative imbalance
- angiogenic deficits
- impaired regenerative capacity
This may explain why some men respond poorly to PDE5 inhibitors despite adequate dosing. The transcriptomic abnormalities highlighted in the study suggest that multi-target therapies may be required, including:
- lifestyle modification
- metabolic control
- anti-inflammatory strategies
- regenerative therapies
- antioxidant support
Treating ED solely by targeting penile smooth muscle relaxation is insufficient when systemic transcriptomic dysfunction persists.
3. New Biomarkers May Be Developed From Deregulated Genes
The differentially expressed genes identified in the study provide fertile ground for:
- molecular biomarkers for early ED detection
- stratification of patients likely to respond to PDE5 inhibitors
- identification of metabolic or inflammatory subtypes of ED
- personalized treatment pathways
Machine learning applied to mRNA expression profiles may eventually predict which patients require vascular, metabolic, or regenerative therapies.
4. Regenerative Medicine Must Account for Inherent Stem Cell Dysfunction
The downregulation of genes related to adipose-derived stem cell (ASC) function offers a crucial insight: not all SVF-derived cells are equal. Men with ED may have SVF cells with inherently limited:
- angiogenic support
- anti-inflammatory capacity
- regenerative signaling
Therefore, autologous cell therapies for ED—while promising—may require sophisticated enhancement techniques such as:
- ex vivo gene editing
- growth factor preconditioning
- mitochondrial optimization
- molecular “rejuvenation” of SVF cells
The study’s mRNA data serve as a roadmap for improving regenerative therapeutics.
5. New Therapies Should Target Multiple Pathways Simultaneously
Future ED therapies may need to move beyond PDE5 inhibition to target:
- inflammatory cytokine networks
- redox homeostasis
- extracellular matrix dynamics
- angiogenic signaling pathways
- stem cell differentiation programs
By addressing the underlying transcriptomic dysregulation rather than only symptomatic vasodilation, treatments can become more durable and comprehensive.
Implications for Research: A New Direction for Erectile Dysfunction Studies
The study has substantial research implications, shifting the field in several important directions.
1. A Systems-Biology Approach to ED
Traditional ED research focused on isolated pathways such as nitric oxide signaling. Whole-genome profiling requires a systems biology lens, integrating interactions between:
- immune system
- extracellular matrix
- metabolic state
- vascular function
- stem cell potential
This holistic perspective enables a deeper understanding of ED’s heterogeneity.
2. SVF as a Research Tissue for ED Studies
The stromal vascular fraction, easily obtained from adipose tissue, provides a practical and informative model for exploring systemic contributions to ED. It avoids the practical limitations of obtaining penile tissue and offers insights relevant to vascular and metabolic health.
This may lead to future research using SVF to study:
- epigenetic changes
- microRNA regulation
- proteomic signatures
- cell-to-cell communication networks
SVF could become a central research platform for early detection and mechanistic exploration.
3. Personalized Medicine in ED
Transcriptomic profiling may eventually be used to classify ED patients into molecular subtypes, such as:
- inflammation-dominant
- fibrosis-dominant
- angiogenesis-deficient
- metabolic-dysfunction–dominant
- stem-cell–impaired
Such classification would revolutionize treatment by aligning therapy with the patient’s dominant molecular phenotype.
A Modern Conceptualization of Erectile Dysfunction: Beyond the Penis
When viewed through the study’s genomic lens, erectile dysfunction emerges as a complex, multilayered disorder deeply embedded in systemic biology. The penis becomes a downstream victim of profound dysregulation occurring in peripheral tissues and circulating molecular networks.
This perspective has three major consequences:
1. ED Is a Cardiometabolic Disease Indicator
The molecular signature in SVF closely mirrors patterns seen in:
- diabetes
- atherosclerosis
- metabolic syndrome
- chronic inflammation
ED may signal early systemic disease even before traditional symptoms arise.
2. ED Is a Disorder of Aging at the Molecular Level
The deregulated pathways reflect hallmarks of biological aging:
- mitochondrial dysfunction
- chronic inflammation
- impaired regeneration
- fibrosis
Thus, ED is not merely age-associated—it is a manifestation of accelerated molecular aging.
3. ED Requires Multidimensional Therapeutic Strategies
Effective long-term management demands:
- metabolic optimization
- anti-inflammatory regulation
- oxidative stress reduction
- restoration of vascular and regenerative capacity
PDE5 inhibitors are a powerful tool, but they cannot correct transcriptomic dysregulation alone.
Conclusion: Whole-Genome Profiling Has Rewritten the Molecular Narrative of ED
The study “Whole genome mRNA expression profiling revealed multiple deregulated pathways in stromal vascular fraction from erectile dysfunction patients” is a landmark contribution to the scientific understanding of ED. Its findings dismantle outdated paradigms and reveal erectile dysfunction as:
- a transcriptomic disorder
- a systemic inflammatory condition
- a disease of dysfunctional regeneration
- a marker of metabolic imbalance
- an early sign of vascular pathology
Most importantly, it demonstrates that ED is not simply the inability to achieve erections—it is the biological expression of deeper molecular dysfunction.
By situating erectile dysfunction within a broader biological context, the study opens doors to innovative diagnostic tools, personalized therapeutic strategies, and regenerative interventions grounded in genomic science.
This research marks a new era in ED: one rooted not only in physiology, but in the language of genes, pathways, and molecular systems.
FAQ
1. Why is the stromal vascular fraction (SVF) relevant to erectile dysfunction?
SVF reflects systemic metabolic, inflammatory, and regenerative states. The study shows that ED patients exhibit transcriptomic abnormalities in SVF, indicating ED is a systemic rather than strictly penile disorder.
2. Does this study mean ED treatments need to change?
Yes. PDE5 inhibitors alone cannot reverse the underlying transcriptomic derangements. ED management must incorporate metabolic, inflammatory, and regenerative strategies.
3. Can transcriptomic profiling improve ED diagnosis?
Potentially. Deregulated genes identified in SVF may serve as biomarkers for early detection, patient stratification, and personalized treatment planning.