Introduction
Erectile dysfunction (ED) is one of the most prevalent disorders affecting men, yet it remains among the most frustrating to manage when conventional therapies fail. Defined as the persistent inability to attain or maintain an erection sufficient for satisfactory sexual performance, ED affects an estimated 150 million men worldwide, with numbers expected to double in the coming decades. Far from being a mere inconvenience, ED has profound effects on quality of life, relationships, and psychological well-being, often serving as a visible marker of underlying vascular or metabolic disease.
The introduction of sildenafil citrate, the first oral phosphodiesterase type 5 (PDE5) inhibitor, revolutionized ED management. It provided a non-invasive, highly effective option for the majority of men, with response rates reaching 70–80% in clinical trials. For those unresponsive to oral therapy, intracavernous injections of vasoactive agents such as prostaglandin E1 (alprostadil) offered another effective, though invasive, alternative. Yet, a stubborn subset of patients—often older men with severe vascular disease, long-standing ED, or complex comorbidities—remained refractory to both strategies.
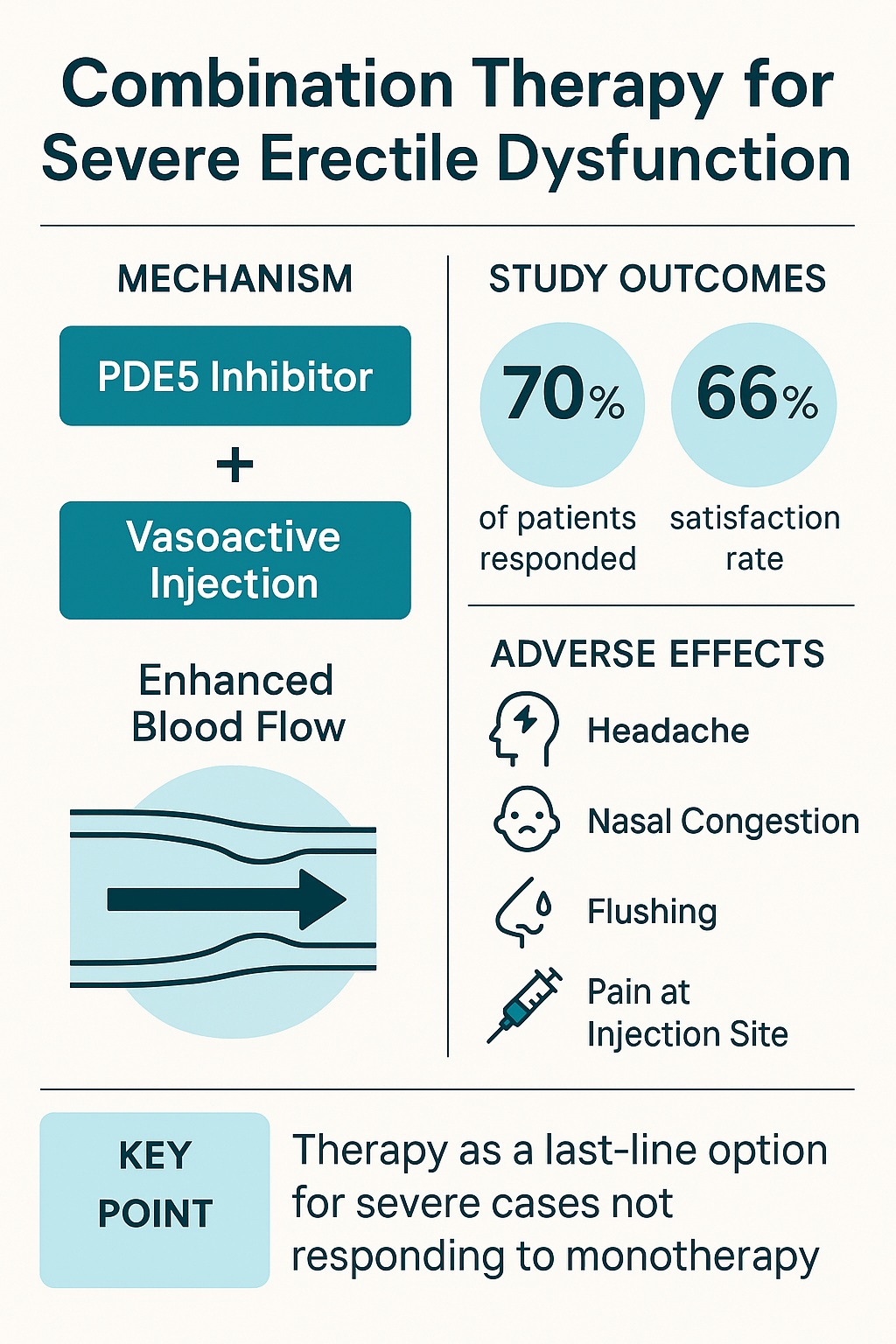
For these patients, the question is no longer how to simplify therapy but how to salvage erectile function at all. The study by Al-Adl and colleagues in 2011 explored this territory, combining chronic low-dose sildenafil with scheduled intracavernous injections of trimix (papaverine, prostaglandin E1, and phentolamine) in men with severe ED unresponsive to either treatment alone. The results, while not universally positive, provided a glimpse into how combined therapy might extend hope to men once considered untreatable.
Understanding Treatment Resistance in ED
To appreciate the logic of combination therapy, one must first understand why monotherapies fail. Sildenafil works by inhibiting PDE5, thereby sustaining cGMP-mediated smooth muscle relaxation in the corpus cavernosum. However, this pathway requires an intact nitric oxide (NO) signal to initiate cGMP production in the first place. In patients with advanced endothelial dysfunction—common in diabetes, hypertension, and atherosclerosis—NO release is impaired, and sildenafil has little substrate to work with.
Intracavernous injections bypass the NO-cGMP pathway altogether by delivering vasoactive agents directly into the penile tissue. Alprostadil increases cyclic AMP, while papaverine and phentolamine relax smooth muscle through complementary mechanisms. Yet, injections too may fail when structural abnormalities, such as fibrosis or venous leak, prevent sustained rigidity.
In essence, refractory ED reflects multifactorial dysfunction: endothelial impairment, cavernosal smooth muscle pathology, and venous incompetence. Addressing one pathway is rarely sufficient. A rational approach, therefore, is to combine therapies that work through different mechanisms—oral sildenafil to enhance cGMP signaling and intracavernous injections to directly relax smooth muscle. The hope is synergy: where one fails, the other compensates, and together they might restore functional erections.
The Study Design
The trial enrolled 40 men with severe erectile dysfunction. All had previously failed maximum tolerated doses of sildenafil and intracavernous prostaglandin E1 monotherapy. Failure was defined stringently: inability to achieve or maintain erections sufficient for penetration in more than 75% of attempts despite appropriate use. This population represented the most challenging clinical scenario—men who had exhausted standard options.
The intervention consisted of daily oral sildenafil 25 mg combined with twice-weekly intracavernous injections of trimix, containing papaverine, prostaglandin E1, and phentolamine in carefully titrated doses. Treatment continued for 8 weeks. Erectile function was assessed using the International Index of Erectile Function (IIEF), penile duplex ultrasound for hemodynamics, and patient/partner satisfaction questionnaires. Side effects were systematically recorded.
The design was pragmatic: rather than a laboratory experiment, it resembled what clinicians might attempt in practice when faced with desperate patients. Its crossover nature—comparing each man’s performance before and after combination therapy—helped highlight true changes attributable to treatment.
The Results: Salvaging Function in the Hardest Cases
After 8 weeks of combined therapy, the findings were cautiously optimistic.
- Responder rate: 70% of men showed significant improvement in erection hardness, duration, and penile hemodynamics. These men moved from non-functional erections to erections adequate for penetration and intercourse.
- Patient satisfaction: Among responders, 66% reported being satisfied with therapy, compared to only 40% of non-responders. This discrepancy underscores that even when erections improve, expectations, comfort, and tolerability influence satisfaction.
- Partner satisfaction: Although not the study’s main focus, reports suggested parallel improvements, reinforcing the relational impact of therapy.
- Adverse effects: Side effects occurred in 43% of participants, including penile pain, flushing, headache, nasal congestion, and dizziness. Importantly, these were tolerable and did not lead to discontinuation in most cases.
- Predictors of non-response: Non-responders tended to be older, with longer ED duration and evidence of veno-occlusive dysfunction on duplex studies, suggesting that structural changes may impose a ceiling beyond which pharmacology cannot compensate.
The study demonstrated that even in men once considered “untreatable,” erectile function can be partially restored through creative combination therapy. While not a miracle cure, it represented progress.
Mechanistic Insights: Why Combination Therapy Works
The synergy between sildenafil and intracavernous injections arises from complementary pathways. Sildenafil enhances cGMP-mediated smooth muscle relaxation but requires NO input. Trimix agents bypass this need, directly inducing smooth muscle relaxation and increasing cavernosal inflow. Together, they provide both the “spark” and the “fuel” for erection.
Hemodynamic studies confirmed this interaction. Penile duplex ultrasound revealed improved arterial inflow and decreased venous leak among responders. It is likely that repeated cavernosal smooth muscle stretching also improved tissue compliance, creating a virtuous cycle of function.
The chronicity of treatment may matter as well. Daily low-dose sildenafil might provide ongoing endothelial support, improving basal NO availability over time. This aligns with evidence from cardiovascular literature suggesting that PDE5 inhibitors exert endothelial protective effects when used chronically. Thus, the regimen may not simply mask dysfunction but modestly rehabilitate vascular health.
Clinical Implications
The immediate implication is that combination therapy can rescue function in men with severe, treatment-resistant ED. For clinicians, this expands the toolkit for a group often left with few options beyond prostheses. Importantly, the regimen remains pharmacological and reversible, avoiding the surgical risks of implants.
For patients, the message is hopeful but realistic. Combination therapy may restore penetration in a majority but not all. Side effects are common though tolerable. Satisfaction depends not only on technical erection hardness but also on psychological acceptance, partner dynamics, and ease of use. Clinicians must set expectations carefully to avoid disappointment.
This strategy is not first-line therapy. It is a salvage approach, appropriate only after failure of optimized monotherapy. Its complexity—daily pills plus regular injections—makes it impractical for casual use. Yet for motivated couples unwilling to accept defeat, it provides a valuable intermediate option before surgery.
Limitations and Considerations
Several caveats temper enthusiasm. The study sample was relatively small (40 men) and drawn from a single center, limiting generalizability. The duration was short (8 weeks), leaving long-term efficacy and safety unknown. The absence of a placebo control group means improvements could partially reflect expectancy effects, though the objective duplex findings support genuine physiological benefit.
The burden of therapy is nontrivial. Twice-weekly injections, even when effective, are daunting for many men and partners. Pain and anxiety surrounding self-injection may limit adherence. Furthermore, adverse effects, though generally mild, occurred in nearly half of participants. Careful monitoring and patient education are mandatory.
Finally, cost and access pose barriers. Trimix is compounded and may not be available universally. Combining it with sildenafil adds expense. For men in resource-limited settings, this regimen may be unrealistic.
Broader Lessons in ED Management
The study offers broader lessons about ED management. First, it underscores the heterogeneity of ED. What works for one man may fail for another, depending on the balance of endothelial health, smooth muscle integrity, and venous competence. Personalized, mechanism-based strategies are essential.
Second, it illustrates the value of combination therapy in complex conditions. Just as hypertension often requires multiple drugs targeting different pathways, severe ED may demand a cocktail approach. The penis, like the heart, does not yield to a single switch but to coordinated restoration of vascular balance.
Third, it highlights the psychological dimension. Even when erections were restored, only two-thirds of responders were satisfied. This gap reveals that treating ED requires attention to relationships, expectations, and mental health alongside pharmacology. Without this, even hemodynamic success may feel like failure.
Conclusion
For men with severe erectile dysfunction unresponsive to both sildenafil and intracavernous prostaglandin monotherapy, hope is not lost. Combination therapy—daily low-dose sildenafil plus scheduled trimix injections—offers meaningful improvement for a majority. Though imperfect, burdensome, and not free of side effects, it represents an important salvage strategy in the escalating hierarchy of ED treatments.
The lesson is that ED, particularly in its severe and resistant forms, rarely has a single solution. Instead, progress comes through layered strategies, creative combinations, and patient-centered care. For clinicians, the key is to recognize when monotherapy has failed and when to offer the next tier of options. For patients, the message is one of cautious optimism: even when first-line treatments fail, persistence, creativity, and partnership can still yield results.
FAQ
1. If sildenafil alone does not work, should men immediately try combination therapy with injections?
No. Combination therapy is a salvage option reserved for men who fail optimized doses of oral PDE5 inhibitors and intracavernous monotherapy. It is not first-line therapy.
2. Are the side effects of combination therapy dangerous?
Most adverse effects—pain, flushing, nasal congestion, headache—are mild and tolerable. Serious complications are rare but require monitoring.
3. What if combination therapy also fails?
In such cases, penile prosthesis implantation remains the definitive solution. Surgical options provide reliable rigidity but carry surgical risks and are irreversible.