Introduction: When Science Meets Convenience
Since its serendipitous discovery in the 1990s, sildenafil has transformed the management of erectile dysfunction (ED), reshaping not only pharmacotherapy but also the social discourse around male sexual health. Once confined to whispered consultations and dimly lit pharmacies, treatment for ED is now part of open clinical conversations. Yet, despite sildenafil’s global success, innovation in its delivery form has lagged behind pharmacologic sophistication.
Most men still take sildenafil as a tablet — effective, yes, but sometimes inconvenient. For patients who value spontaneity or struggle with swallowing pills, an orally disintegrating strip (ODS) might offer the perfect blend of efficacy and ease. In theory, the ODS formulation allows the drug to dissolve on the tongue within seconds, bypassing the need for water and possibly shortening the onset of action.
A research team from Mahidol University, Thailand, took this hypothesis into the clinic. Their prospective, randomized, controlled crossover trial compared traditional sildenafil tablets with a novel ODS formulation. The goal was clear: to determine whether convenience could coexist with pharmacologic potency — and whether the new strip could hold its ground against the tablet that defined a therapeutic era.
Understanding the Foundations: How Sildenafil Works
At its molecular core, sildenafil is a phosphodiesterase type 5 (PDE5) inhibitor. During sexual stimulation, nitric oxide (NO) released in penile tissue activates guanylate cyclase, which increases cyclic guanosine monophosphate (cGMP) levels. This biochemical cascade induces smooth muscle relaxation, leading to increased blood flow into the corpus cavernosum — the essence of an erection.
However, PDE5 rapidly degrades cGMP, terminating the erection prematurely. By inhibiting PDE5, sildenafil prolongs cGMP activity and thus sustains erectile rigidity. This mechanism is elegant and efficient, but its pharmacokinetics — specifically absorption, metabolism, and onset — depend heavily on the delivery method and gastrointestinal conditions.
Conventional sildenafil tablets are absorbed through the gastrointestinal tract, with a Tmax of 30–60 minutes. High-fat meals can delay absorption, while hepatic metabolism through CYP3A4 and CYP2C19 determines elimination. This interplay means that even minor variations in digestion, alcohol intake, or meal timing can alter efficacy and timing — a potential barrier to spontaneous intimacy.
Enter the orally disintegrating strip — a formulation designed to bypass gastric variables and offer a faster, more predictable onset. But can this new form match the gold standard in performance and safety?
The Study: Crossover Design Meets Clinical Precision
The Thai study enrolled 120 men diagnosed with erectile dysfunction, ranging in age from their late 40s to mid-70s (mean: 64.5 years). The crossover design ensured that every participant experienced both formulations, reducing interindividual variability — a methodological strength in trials involving subjective outcomes like sexual performance.
Participants were randomized into two groups:
- Arm 1: Began with sildenafil ODS (Hart-S, 50 mg per strip; two strips before intercourse) for 8 weeks, followed by a 4-week washout, then 8 weeks on the conventional tablet (100 mg).
- Arm 2: Started with the tablet regimen and later switched to ODS after washout.
Throughout 8 visits over 20 weeks, participants completed validated questionnaires:
- The abridged International Index of Erectile Function (IIEF-5) — a psychometric tool quantifying erection quality, satisfaction, and sexual confidence.
- The Erection Hardness Score (EHS) — a patient-reported scale ranging from 1 (“penis does not enlarge”) to 4 (“completely hard and fully rigid”).
The study also assessed onset and duration of action, adverse effects, and patient preference, thereby capturing not just pharmacologic efficacy but also real-world usability.
Results: Two Formulations, One Outcome
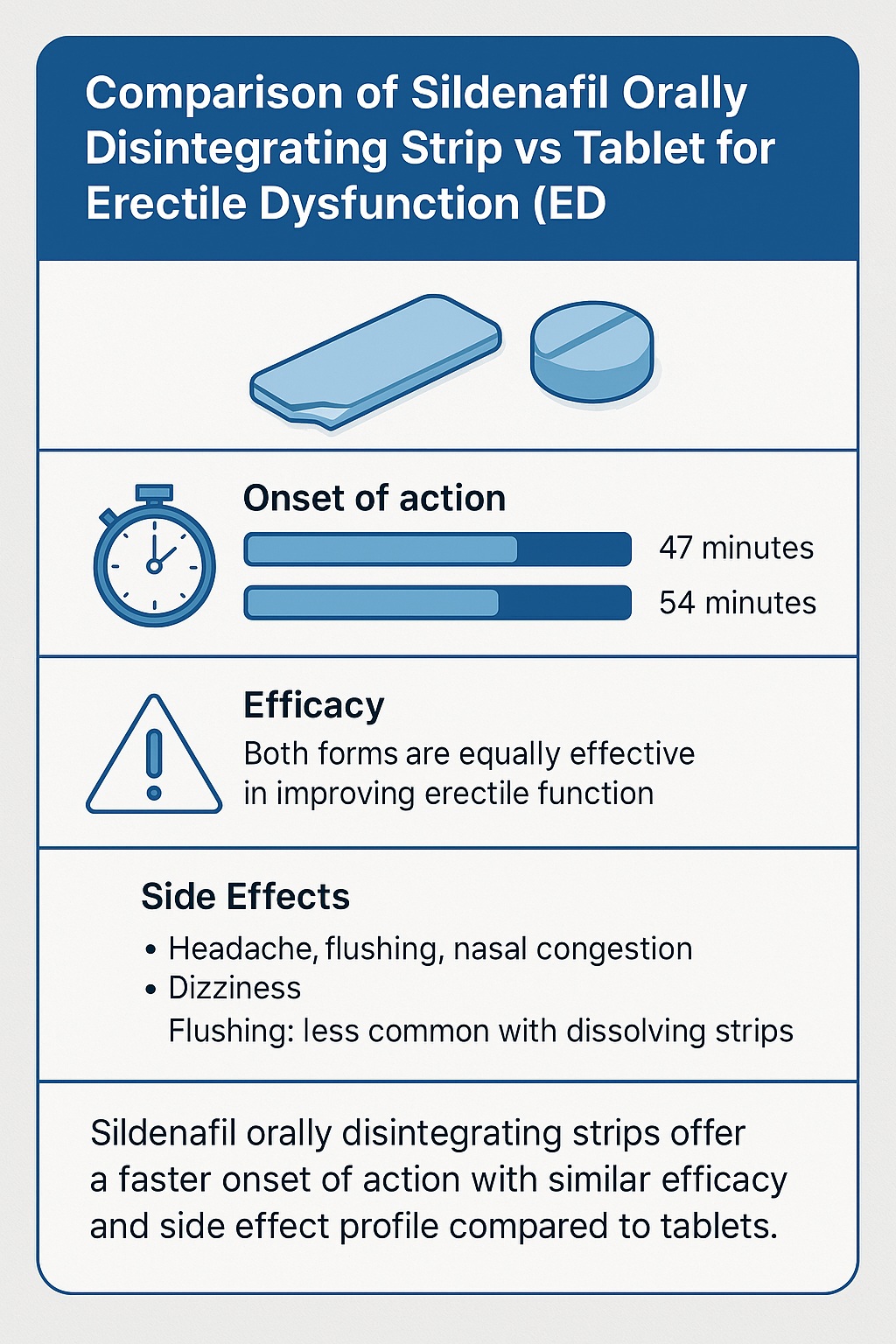
The headline result is elegantly simple: both sildenafil formulations were equally effective in improving erectile function. After treatment, mean IIEF-5 scores increased from about 14.5 (mild-to-moderate ED) to 18 (mild ED) — a clinically meaningful gain that shifted most patients into a functional sexual category.
Likewise, EHS values improved from approximately 2.6 to over 3.0, indicating a transition from erections insufficient for penetration to those firm enough for satisfactory intercourse.
The improvements were consistent across age groups and comorbidities. Neither diabetes, hypertension, nor benign prostatic hyperplasia significantly affected efficacy — a notable finding given that these are among the most common contributors to ED.
A Slight Edge in Onset
While the difference wasn’t statistically significant, the ODS formulation demonstrated a 7.1-minute faster onset of action compared to the tablet (47.1 vs. 54.2 minutes). This seemingly modest gap may have tangible meaning for patients seeking spontaneity. After all, in the emotional calculus of intimacy, minutes can matter.
Duration of effect was also similar — around 85–90 minutes — reinforcing that the strip maintains comparable pharmacodynamics to the tablet.
Adverse Events: Familiar, Mild, and Manageable
Both formulations shared a nearly identical safety profile. The most common side effects included:
- Headache (≈12%)
- Flushing (slightly more frequent in tablet users)
- Nasal congestion
- Dizziness or mild visual disturbance
No serious or life-threatening adverse events occurred. Interestingly, the ODS users reported fewer flushing episodes, possibly due to altered absorption kinetics or reduced systemic vasodilation.
At the study’s end, patient preferences were evenly split — 47% favored the ODS for its convenience and taste, while 53% preferred tablets for familiarity. In medicine, a tie often means success for the newcomer.
The Science of Dissolution: Why Form Matters
The ODS technology represents a subtle yet meaningful advance in drug delivery. Each strip contains sildenafil embedded within a thin, polymeric matrix that rapidly dissolves on contact with saliva, releasing the drug for buccal and sublingual absorption. This route partially bypasses first-pass hepatic metabolism, potentially offering higher bioavailability.
From a pharmacologic perspective, orodispersible delivery can:
- Enhance patient compliance — especially among older adults or those with dysphagia.
- Accelerate onset by enabling absorption through the oral mucosa.
- Reduce gastrointestinal dependency, making timing with meals less critical.
- Improve discretion, as administration requires no water or pill swallowing.
For ED, where timing, privacy, and spontaneity intersect, these benefits are not trivial. Even without statistically significant superiority, the psychological and practical advantages of ODS formulations may prove decisive for some patients.
The Context: ED in Aging and Comorbidity
Erectile dysfunction affects an estimated 322 million men worldwide by 2025, with prevalence rising sharply with age and cardiometabolic disease. In the Thai population studied, nearly 56% had hypertension, 52% dyslipidemia, and 48% benign prostatic hyperplasia — a microcosm of the global demographic shift toward multimorbidity.
Sildenafil, by improving endothelial function and penile blood flow, addresses not only sexual health but also signals vascular health more broadly. Studies consistently show that ED is an early marker of systemic endothelial dysfunction, often preceding overt cardiovascular disease by years.
However, standard tablet-based regimens may not suit all patients, particularly those with polypharmacy or impaired gastric absorption. Thus, the emergence of ODS formulations is part of a broader trend in personalized pharmacotherapy, where drug design aligns with patient physiology and lifestyle.
Patient Psychology and Preference: Beyond Pharmacology
While pharmacokinetics matter, psychological readiness is equally critical in ED treatment. Many men associate tablets with illness — a reminder of aging or dependency — whereas a dissolving strip can feel more natural, less clinical, and more spontaneous.
Moreover, ODS use eliminates the ritual of swallowing a pill before intimacy, which some couples find disruptive. As one might humorously note, the less medical an encounter feels, the more romantic it becomes.
In the Thai study, nearly half the participants preferred the strip — not because it worked better, but because it fit better into their lives. That subtle distinction often determines long-term adherence in sexual medicine.
The Pharmacoeconomic Angle: Cost and Accessibility
Currently, ODS formulations are not yet widely available in Thailand or many low- and middle-income regions. Cost comparisons were not included in the trial, but manufacturing ODS involves specialized technology — solvent casting, polymer coating, and flavor stabilization — which could increase retail prices initially.
However, mass production and generic competition are likely to narrow this gap. If patient adherence and satisfaction improve with ODS, the long-term cost-effectiveness could be favorable, given that adherence directly correlates with therapeutic success and reduced psychological burden.
Clinical Implications: How Should Physicians Use This Information?
From a clinician’s standpoint, the findings invite pragmatic optimism rather than revolution. The ODS form is not superior to the tablet in efficacy but stands as a clinically equivalent alternative with added convenience.
In practice, this means:
- For patients who experience difficulty swallowing, the ODS is ideal.
- For those seeking faster, more discreet administration, ODS offers psychological ease.
- For those satisfied with tablets, there is no medical need to switch.
In patients who report flushing or gastrointestinal discomfort with tablets, the strip may provide improved tolerability. However, clinicians should emphasize that both forms require sexual stimulation to be effective — a point still frequently misunderstood.
Limitations and Lessons from the Study
Every study has its boundaries. The Thai trial’s limitations include:
- Lack of a placebo arm, since withholding PDE5 inhibitors in diagnosed ED would be unethical and unappealing to participants.
- Open-label design, unavoidable due to the obvious physical differences between strip and tablet.
- Self-reported timing of onset and duration, which introduces subjectivity.
- Limited geographic scope, focusing solely on Thai men, which may limit generalizability.
Yet, these limitations do not undermine the study’s strength — its crossover design, which minimizes interindividual variability, and its use of validated tools (IIEF-5 and EHS). The absence of serious adverse events reinforces the safety of both formulations under real-world conditions.
The Broader Perspective: Where Innovation in ED Therapy Is Headed
The development of sildenafil ODS aligns with a broader pharmaceutical evolution — one that prioritizes user experience alongside efficacy. Similar ODS systems have been explored for drugs like zolmitriptan (for migraines) and risperidone (for schizophrenia), emphasizing portability, convenience, and adherence.
In sexual medicine, where emotional and relational dynamics intersect with pharmacology, delivery forms that reduce anxiety and increase spontaneity can profoundly influence outcomes. The success of sildenafil ODS might encourage innovation in other PDE5 inhibitors — tadalafil and vardenafil — paving the way for a new generation of “smart” dissolving films.
Future studies may explore microdose titration, dual-acting films (combining PDE5 inhibition with nitric oxide donors), or flavor-optimized patient-specific formulations. In other words, the next frontier of ED treatment may lie less in molecules and more in how we deliver them.
Conclusion: A Modern Twist on a Classic Drug
The sildenafil orally disintegrating strip represents an evolution, not a reinvention, of ED therapy. It delivers equivalent efficacy and safety to the conventional tablet, with a modestly faster onset and fewer flushing episodes. While statistically similar, these small differences can translate into meaningful real-world benefits — particularly for patients valuing discretion and spontaneity.
As medicine increasingly embraces patient-centered design, the ODS form exemplifies how innovation can reside not in chemistry, but in experience. The little blue pill has met its nimble, dissolving cousin — and for many men, that’s progress worth celebrating.
FAQ: Sildenafil Orally Disintegrating Strips
1. Do sildenafil dissolving strips work as well as tablets?
Yes. Clinical evidence shows that orally disintegrating strips are as effective as conventional tablets in improving erectile function, with comparable safety and duration of action.
2. Are the dissolving strips faster-acting than regular sildenafil?
Slightly. On average, the onset of action is about 7 minutes faster, which may feel more spontaneous for some users, though the difference is not statistically significant.
3. Who should consider switching to the strip formulation?
Patients who have difficulty swallowing pills, prefer a more discreet or convenient method, or experience flushing with tablets may benefit most from the orally disintegrating strip.