Introduction: When Science Meets Sleep
Erectile dysfunction (ED) remains one of the most discussed, yet misunderstood, conditions in male sexual medicine. Often simplified as a mechanical failure or a symptom of aging, ED is, in truth, a multifactorial disorder involving neurovascular, hormonal, and psychological interplay. It is both a barometer of vascular health and a mirror reflecting psychological resilience.
Among the armamentarium of diagnostic and therapeutic approaches, phosphodiesterase type 5 inhibitors (PDE5i)—notably sildenafil—have transformed management paradigms. Yet even this pharmaceutical marvel has its limitations: not every man responds to the “blue pill.” Roughly 30% of patients exhibit suboptimal or absent response, raising a critical clinical question—can we predict who will benefit before prescribing?
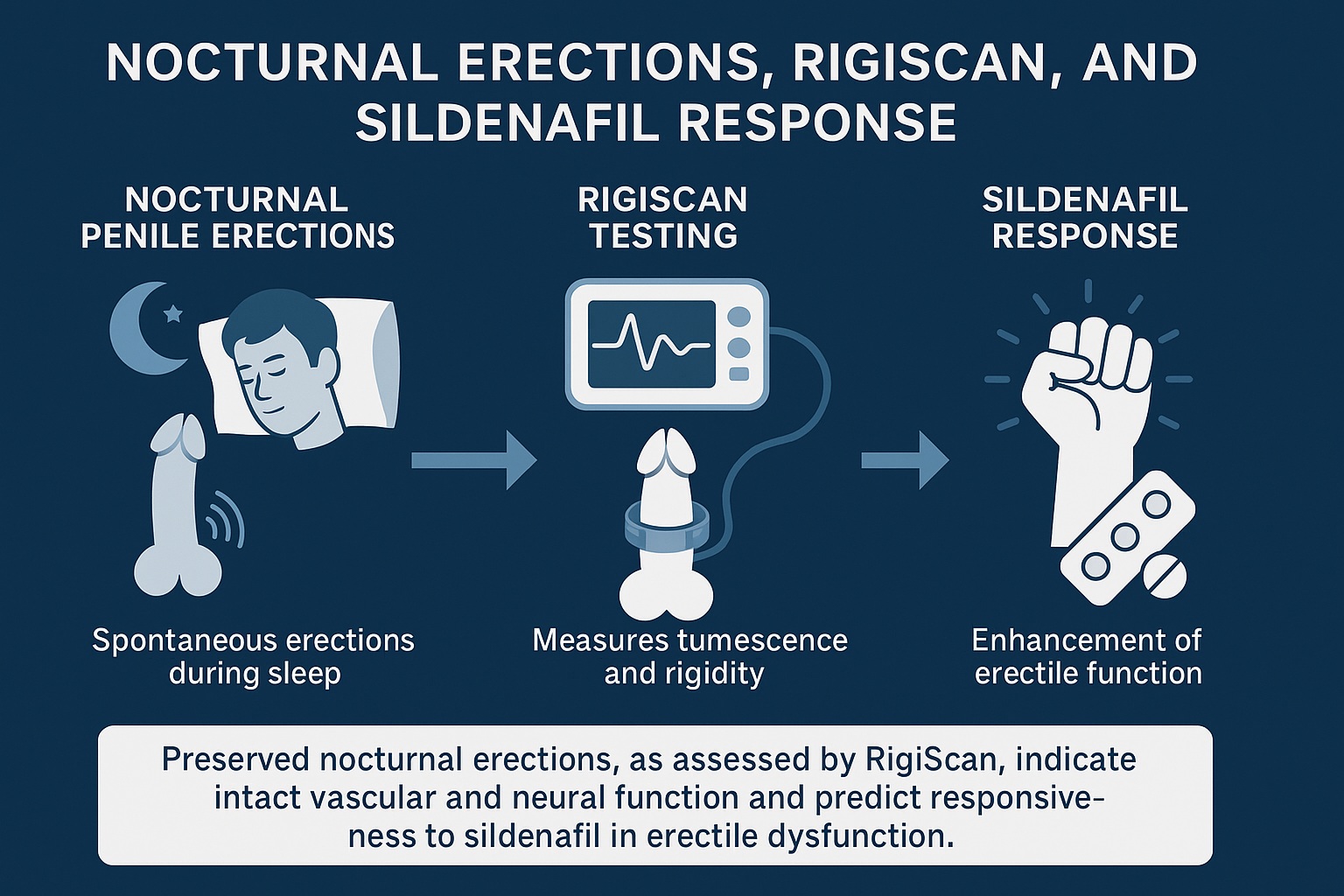
The study by Elhanbly and colleagues (2018) addresses this question with elegant simplicity: by examining the diagnostic role of nocturnal penile erections (NPEs) measured using the RigiScan device. The authors hypothesize that assessing a man’s erections during sleep can predict how he will respond to sildenafil in waking life. A poetic idea indeed—nighttime physiology guiding daytime therapy.
The Science of the Sleeping Erection
It may sound whimsical, but nocturnal penile erections are one of the most physiologically robust phenomena in male biology. Healthy men, regardless of age, typically experience three to five erections per night, each lasting 20–40 minutes and occurring during rapid eye movement (REM) sleep.
The neurophysiology of NPEs is distinct from that of psychogenic or reflexogenic erections. While waking erections rely on cortical and sensory stimuli, nocturnal erections are largely autonomic, driven by cholinergic and nitric oxide-mediated mechanisms independent of conscious arousal. This makes them a perfect indicator of organic erectile integrity—the vascular and neurological competence of the penile apparatus.
Thus, when ED patients retain normal NPEs, it suggests that the physical architecture is intact and the problem may lie in psychogenic or situational factors. Conversely, impaired NPEs indicate organic pathology—endothelial dysfunction, neuropathy, or vascular insufficiency.
In clinical practice, evaluating nocturnal erections offers a window into distinguishing psychogenic from organic ED—a distinction that profoundly influences treatment planning and prognostic counseling.
The RigiScan Device: Quantifying the Unseen
Enter RigiScan, a compact marvel of medical engineering. This portable device records penile tumescence (size) and rigidity through strain gauge technology during sleep. Two loops—one at the base, another at the tip—measure real-time fluctuations in circumference and stiffness, translating them into precise digital metrics.
RigiScan doesn’t merely capture presence or absence of erection—it quantifies it. Among its key parameters:
- Erection Hardness (% rigidity) – percentage of maximal rigidity achieved.
- Duration of rigidity ≥60% – duration sufficient for penetrative intercourse.
- Number and frequency of nocturnal erections – indicating overall vascular activity.
- Tumescence changes – tracking penile volume variation through the night.
For clinicians, these data act as a diagnostic compass: distinguishing psychogenic ED (where NPEs remain normal) from vascular or neurogenic forms (where NPEs are diminished or absent).
Study Design: Retrospective Precision
Elhanbly et al. conducted a retrospective observational study involving 66 men with clinically diagnosed erectile dysfunction. The goal was to determine whether RigiScan-measured NPE parameters could predict sildenafil responsiveness.
The methodology was straightforward yet elegant:
- Each participant underwent baseline clinical evaluation, including medical history, IIEF (International Index of Erectile Function), and hormonal profiling.
- Nocturnal penile tumescence and rigidity (NPTR) testing was performed for two consecutive nights using RigiScan.
- Participants were then prescribed sildenafil citrate (50–100 mg) for a trial period, with response defined by both subjective improvement (IIEF score rise ≥5 points) and objective sexual performance.
- Data were analyzed to correlate RigiScan parameters with treatment outcomes.
The patients were divided into two groups:
- Responders (n=48) – significant erectile improvement with sildenafil.
- Non-responders (n=18) – minimal or no improvement.
Key Findings: Nighttime Predicts Daytime
The results were striking and statistically robust. Among the 66 participants:
- 72.7% responded favorably to sildenafil therapy.
- 27.3% failed to achieve satisfactory erections despite optimal dosing.
When RigiScan data were compared between groups, patterns emerged that illuminated the physiology behind these outcomes.
1. Rigidity at the Tip and Base
Responders exhibited significantly higher mean rigidity at both the penile tip and base compared to non-responders.
- Responders: mean tip rigidity ≈ 65%, base rigidity ≈ 75%.
- Non-responders: mean tip rigidity ≈ 35%, base rigidity ≈ 40%.
This suggests that adequate nocturnal rigidity correlates strongly with vascular integrity—the very mechanism sildenafil enhances by promoting nitric oxide-mediated smooth muscle relaxation.
2. Duration of Functional Erections
In responders, the duration of rigidity ≥60% was notably longer—often exceeding 10 minutes per episode, versus less than 5 minutes among non-responders. This parameter closely predicts real-world sexual performance potential.
3. Frequency of Nocturnal Erections
Responders also had a greater number of NPE episodes per night. The cumulative evidence reinforces that robust nocturnal erectile activity signals preserved penile vasculature capable of pharmacologic stimulation.
The Physiology Behind Prediction
Why do nocturnal erections predict sildenafil response so reliably? The answer lies in shared pathophysiology.
Both NPEs and sildenafil-induced erections depend on:
- Endothelial nitric oxide synthase (eNOS) activity.
- cGMP-mediated smooth muscle relaxation.
- Intact cavernosal vascular responsiveness.
If the neurovascular machinery is intact, nocturnal erections occur spontaneously—and such tissue will predictably respond to PDE5 inhibition. Conversely, if nocturnal erections are blunted or absent, it suggests endothelial impairment or fibrosis—conditions in which even maximal pharmacologic vasodilation cannot restore function.
Thus, RigiScan serves as a functional stress test for penile circulation—a noninvasive predictor of therapeutic success.
Clinical Implications: From Diagnostics to Decision-Making
The implications of these findings are profound for clinical practice. Erectile dysfunction is often treated empirically: a PDE5 inhibitor is prescribed, and success or failure is determined by patient feedback. This trial-and-error approach can be inefficient, costly, and psychologically discouraging.
Integrating RigiScan-based NPE assessment offers several advantages:
- Predictive Accuracy: Clinicians can estimate the likelihood of sildenafil success before therapy, avoiding unnecessary medication trials.
- Diagnostic Clarity: Differentiating psychogenic from organic ED aids in targeted interventions—psychotherapy vs. pharmacotherapy vs. vascular workup.
- Treatment Personalization: Non-responders can be promptly directed toward alternative treatments—vacuum erection devices, intracavernosal injections, or even penile prostheses.
In this way, RigiScan bridges diagnostic precision with therapeutic strategy—a hallmark of personalized medicine.
Beyond Sildenafil: Broader Diagnostic Horizons
While the study focuses on sildenafil, the principle extends to all PDE5 inhibitors—tadalafil, vardenafil, and avanafil. Each shares the same fundamental mechanism: amplification of nitric oxide signaling. Thus, preserved NPEs should predict responsiveness across the PDE5 inhibitor class.
Moreover, RigiScan findings have diagnostic applications beyond pharmacologic prediction:
- Post-prostatectomy evaluation – distinguishing neuropathic from vascular dysfunction.
- Endocrine disorders – assessing hypogonadism-related changes in erectile quality.
- Diabetes mellitus – early detection of subclinical vascular compromise.
In essence, the nocturnal erection becomes not merely a symptom but a biological biomarker—a natural report card of endothelial vitality.
Limitations and Considerations
Like all scientific endeavors, this study carries methodological constraints that temper its generalizability.
- Retrospective Design: The analysis, though insightful, is inherently limited by retrospective data collection. Future prospective studies could better establish causality.
- Sample Size: Sixty-six patients, while statistically valid, represents a modest cohort. Larger, multicentric trials would strengthen predictive validity.
- Single-Dose Response: Sildenafil responsiveness was measured after limited exposure; some “non-responders” may have required dose titration or repeated trials.
- Psychological Confounders: NPEs assess organic capacity, not psychogenic inhibition. Men with anxiety, relational issues, or depression may retain normal NPEs but still experience ED in real-world contexts.
Nevertheless, within these boundaries, the data remain compelling—particularly for clinicians navigating the diagnostic gray zones of ED management.
The Subtle Art of Differentiation: Psychogenic vs. Organic ED
The real brilliance of this research lies in reviving an old but underused diagnostic distinction: psychogenic vs. organic erectile dysfunction.
In psychogenic ED, the penile vasculature and nerves are intact, but psychological barriers—performance anxiety, relationship stress, depression—disrupt cortical initiation of erection. These men typically exhibit normal NPEs and respond dramatically to PDE5 inhibitors or psychotherapy.
Conversely, in organic ED—often due to diabetes, atherosclerosis, or pelvic nerve injury—NPEs are reduced or absent, and pharmacologic response is correspondingly limited.
In this sense, the night does not lie. What the RigiScan reveals during REM sleep can guide therapy during waking hours with surprising precision.
Integrating RigiScan Into Clinical Workflow
Incorporating RigiScan testing into routine urological or sexual medicine evaluation can streamline diagnostic algorithms. A pragmatic workflow might include:
- Initial assessment – detailed medical, psychological, and sexual history with IIEF scoring.
- Basic labs – hormonal profile (testosterone, prolactin, LH, fasting glucose).
- NPE testing – two-night RigiScan evaluation to assess baseline erectile function.
- Therapeutic trial – PDE5 inhibitor prescribed only if NPEs are adequate.
- Alternative pathway – if NPEs are poor, investigate vascular or neuropathic etiologies.
This evidence-based sequence saves time, optimizes resources, and enhances patient confidence by aligning therapy with physiological reality.
The Psychological Dimension: Managing Expectations
An often-overlooked element of ED therapy is expectation management. Patients approach PDE5 inhibitors with inflated hopes, influenced by cultural narratives of instant and universal efficacy. When therapy fails, disappointment can compound performance anxiety, leading to a vicious cycle of psychological inhibition.
RigiScan testing allows physicians to discuss prognosis transparently. If nocturnal erections are robust, the patient can be reassured of likely pharmacologic success. If diminished, counseling can emphasize vascular or lifestyle modification rather than pharmacologic dependence.
In this way, data-driven reassurance replaces speculation, and patient trust deepens.
The Broader Meaning: Erectile Function as a Health Barometer
ED has long been recognized as a sentinel symptom for systemic vascular disease. Impaired endothelial function in penile arteries often precedes coronary or carotid pathology. Thus, assessing erectile function—day or night—offers clinicians an early warning system for broader cardiovascular risks.
The RigiScan’s quantification of nocturnal erection patterns could therefore extend beyond sexual medicine, serving as a noninvasive proxy for vascular health. Regular assessment might even one day become part of cardiovascular risk stratification protocols—a vision where sleep-derived data inform preventive cardiology.
Conclusion: Listening to the Language of the Night
The study by Elhanbly et al. elegantly reminds us that human physiology communicates its truths in subtle ways. The nocturnal erection—spontaneous, involuntary, and rhythmically recurring—is not merely an artifact of sleep but a diagnostic signal, revealing the integrity of vascular, neural, and hormonal systems.
By harnessing the RigiScan to interpret this language, clinicians can predict who will benefit from sildenafil, who needs deeper investigation, and who may require alternative therapy. In doing so, we transform a subjective complaint into an objective, measurable, and predictable physiological process.
In short, nocturnal erections are nature’s own stress test—quiet, revealing, and clinically invaluable.
FAQ: Nocturnal Erections, RigiScan, and Sildenafil Response
1. What exactly does RigiScan measure?
RigiScan quantifies penile tumescence (size increase) and rigidity during sleep, providing data on frequency, duration, and strength of nocturnal erections. It helps differentiate between psychogenic and organic erectile dysfunction.
2. Can normal nocturnal erections guarantee sildenafil success?
While not an absolute guarantee, preserved nocturnal erections strongly predict positive sildenafil response. It means the penile vasculature and neural pathways are intact and responsive to nitric oxide-mediated vasodilation.
3. If nocturnal erections are poor, does that mean sildenafil will fail?
Not necessarily, but chances are reduced. Poor NPEs suggest underlying organic dysfunction (vascular, neuropathic, or fibrotic), which may require alternative treatments or combination therapy.