Introduction
Erectile dysfunction (ED) represents one of the most common conditions encountered in men as they age. Defined as the persistent inability to achieve or maintain an erection sufficient for satisfactory sexual performance, ED is far from a trivial inconvenience. It compromises intimacy, self-esteem, and quality of life, while often signaling underlying systemic pathology such as diabetes, cardiovascular disease, or hormonal imbalance.
Among the multitude of contributing factors, declining testosterone levels with age—often termed late-onset hypogonadism—deserve particular attention. Although not all cases of ED are attributable to androgen deficiency, a critical threshold of testosterone is often necessary to sustain sexual function. This threshold involves not only libido and central arousal but also the peripheral mechanisms of penile erection, including nitric oxide (NO) production and smooth muscle responsiveness.
Phosphodiesterase type 5 inhibitors (PDE5Is), such as sildenafil, revolutionized ED therapy by enhancing the NO–cGMP pathway. Yet a substantial subset of patients remains unresponsive to these agents. Clinical observations suggest that testosterone supplementation can restore responsiveness in hypogonadal men. This raises an important clinical question: should testosterone therapy be considered not merely as hormone replacement but as a key adjunct in ED management?
The Androgen Connection: Testosterone and Sexual Function
Testosterone is the primary male sex hormone, secreted mainly by Leydig cells in the testes. Its functions extend well beyond the reproductive system, influencing mood, metabolism, bone density, muscle mass, and cardiovascular health. In the sexual domain, testosterone regulates libido, erectile physiology, and overall sexual satisfaction.
Experimental suppression of testosterone in eugonadal men predictably reduces sexual desire and activity. Severe hypogonadism may cause ED by altering penile structure and impairing vasodilatory pathways. Importantly, while some men maintain erections despite very low testosterone, many require a minimal androgenic environment to sustain both interest and erectile capacity.
With aging, serum testosterone levels decline gradually, often leading to symptomatic late-onset hypogonadism. Its manifestations—fatigue, reduced muscle strength, mood changes, decreased libido, and ED—reflect testosterone’s pervasive physiological influence. Importantly, ED may serve as the earliest and most distressing symptom, bringing patients to clinical attention.
Insights from Animal Studies
Animal models provide valuable mechanistic insights into the role of androgens in erectile physiology. Castration in rats produces ED, characterized by reduced intracavernosal pressure, diminished smooth muscle content, and venous leakage. At the cellular level, castration induces apoptosis in penile tissue, specifically within the corpora cavernosa. Testosterone replacement reverses these changes, promoting DNA synthesis and cell survival.
Furthermore, studies demonstrate that androgen deficiency reduces nitric oxide synthase (NOS)-containing nerves within erectile tissue. This finding suggests that testosterone regulates neuronal nitric oxide synthase (nNOS), a critical enzyme for initiating erections. Castrated rats exhibit attenuated erectile responses to neural stimulation, an effect corrected by testosterone supplementation.
Interestingly, some vasodilatory mechanisms in the penis remain androgen-regulated but independent of nitric oxide. For example, testosterone-treated rats retain intracavernosal pressure responses even under NOS inhibition, indicating multiple androgen-sensitive pathways. These findings underscore the hormone’s multifaceted role in erectile physiology—supporting structural integrity, neuronal signaling, and smooth muscle function.
Translating Evidence to Humans
While animal studies establish causality, human data present a more nuanced picture. Not all hypogonadal men suffer from ED, and not all ED patients are hypogonadal. The variability reflects differences in individual sensitivity to testosterone, the presence of comorbidities, and the multifactorial nature of erectile dysfunction.
Nevertheless, clinical evidence consistently demonstrates that testosterone replacement improves libido, sexual activity, and frequency of erections in hypogonadal men. In some studies, up to 60% of patients report significant improvement, while others show modest gains. These variable results emphasize the importance of patient selection and realistic counseling.
Importantly, ED in men with normal testosterone may not improve with supplementation. Thus, testosterone therapy should not be considered a universal remedy but rather a targeted intervention for men with biochemical and clinical evidence of androgen deficiency.
Testosterone and the Nitric Oxide Pathway
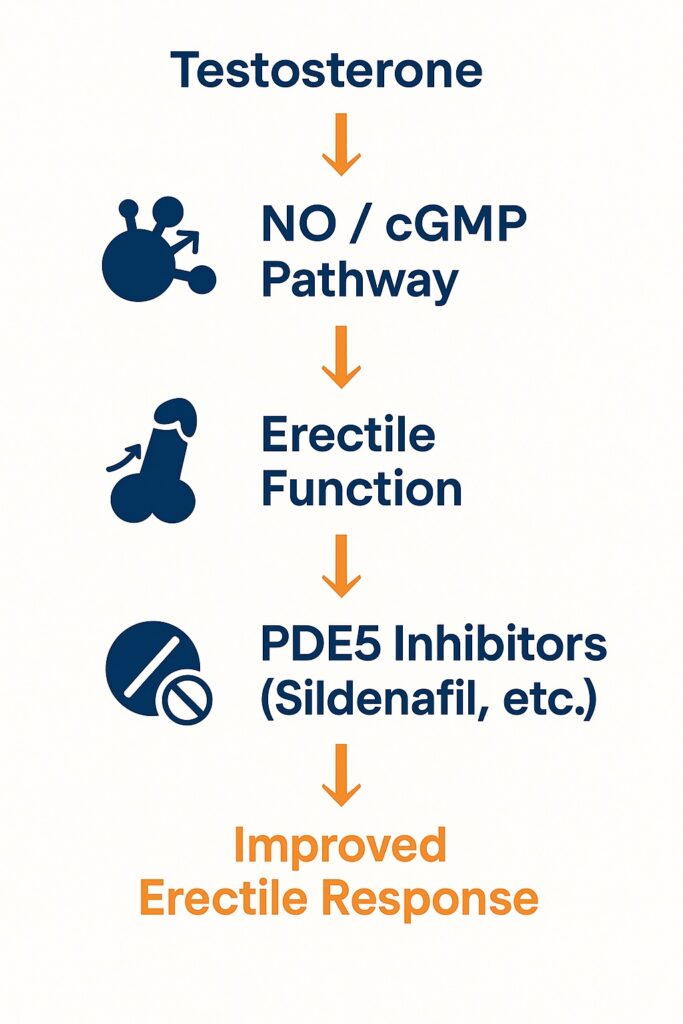
The NO–cGMP pathway is central to penile erection. Sexual stimulation triggers release of NO from both endothelial cells and neuronal endings within the corpora cavernosa. NO activates guanylyl cyclase, increasing cGMP levels, which reduce intracellular calcium and induce smooth muscle relaxation. Blood fills the sinusoidal spaces, compressing venules against the tunica albuginea and producing erection.
Testosterone appears to enhance this cascade at multiple levels. It stimulates nNOS expression, maintains endothelial function, and preserves smooth muscle responsiveness. In hypogonadal states, reduced NO availability and impaired cGMP signaling compromise erectile physiology, rendering PDE5 inhibitors less effective. This explains why some men fail sildenafil therapy until testosterone is restored to adequate levels.
Thus, testosterone provides the biochemical foundation upon which PDE5Is can act effectively. Without sufficient androgen support, pharmacological amplification of cGMP is insufficient to produce clinically meaningful erections.
Testosterone Therapy: Modalities and Evolution
Testosterone replacement has evolved significantly over the past decades. Early regimens involved intramuscular injections of testosterone enanthate or cypionate. While effective, these formulations produced fluctuating serum levels, leading to alternating peaks and troughs that caused mood swings and variable symptom control.
Transdermal systems were later introduced. The first scrotal patches delivered physiological testosterone but caused supraphysiological dihydrotestosterone levels and required scrotal shaving, limiting patient acceptance. Non-scrotal patches improved convenience but were plagued by skin irritation and poor adherence.
Modern preparations now include transdermal gels (such as Testogel® and AndroGel®), which provide stable serum testosterone with daily application. These formulations rapidly restore hormone levels, improve sexual function, and enhance mood with relatively few side effects. Flexible dosing and minimal skin reactions have made gels the preferred option for many patients.
Other modalities—such as long-acting intramuscular injections, subcutaneous pellets, and oral undecanoate—offer alternatives tailored to patient preferences and clinical needs. Regardless of delivery system, the goal remains consistent: restore testosterone to mid-normal physiological levels and relieve symptoms of hypogonadism.
Combination Therapy with PDE5 Inhibitors
The introduction of PDE5 inhibitors transformed ED management. Drugs like sildenafil enhance erection by preventing cGMP degradation in the corpora cavernosa. However, their efficacy depends on adequate NO and cGMP synthesis, processes that are androgen-dependent.
Clinical studies confirm the synergy between testosterone and PDE5Is. In hypogonadal men unresponsive to sildenafil alone, supplementation with testosterone frequently restores responsiveness. For example, in one multicenter trial, men with low to low-normal testosterone and refractory ED were randomized to testosterone gel plus sildenafil versus placebo gel plus sildenafil. After 12 weeks, the combination group demonstrated significant improvements in erectile function, orgasmic satisfaction, and overall sexual satisfaction. Importantly, testosterone levels rose from subnormal to physiological ranges, correlating with clinical response.
Another study in diabetic men highlighted the same principle: testosterone supplementation increased libido and restored sildenafil responsiveness in a substantial proportion of non-responders. These findings underscore the need to evaluate testosterone status in any man who fails PDE5I monotherapy.
Practical Considerations in Clinical Practice
The evaluation of men with ED should include a thorough history, physical examination, and laboratory testing. Screening for hypogonadism is particularly important in men with decreased libido, low energy, or poor PDE5I response. Morning total testosterone measurement remains the standard, with repeat testing to confirm low values. Free testosterone measurement may be helpful in borderline cases.
When hypogonadism is confirmed, testosterone therapy should be considered, especially if symptoms are present. Prior to initiation, clinicians must counsel patients on potential risks and monitor for contraindications such as prostate cancer, severe sleep apnea, or polycythemia. Regular follow-up is essential, with periodic assessment of hematocrit, prostate-specific antigen (PSA), and clinical response.
Combination therapy with PDE5Is should be individualized. Not all patients require it, but in those with persistent ED despite adequate testosterone replacement, PDE5Is can provide additive benefit. The therapeutic sequence—testosterone first, followed by PDE5Is if needed—is a rational approach that maximizes efficacy while minimizing unnecessary drug exposure.
Challenges and Controversies
Despite clear evidence of benefit, testosterone therapy remains surrounded by controversy. Concerns about cardiovascular risk, prostate cancer stimulation, and misuse as a lifestyle drug have tempered enthusiasm. While current evidence suggests that testosterone replacement is safe when monitored appropriately, long-term data remain limited.
Another challenge lies in patient expectations. Some men view testosterone as a quick fix for all symptoms of aging, while others resist therapy due to misconceptions about safety. Physicians must navigate these perspectives with balanced education, emphasizing both benefits and limitations.
Finally, variability in diagnostic criteria complicates clinical decision-making. The threshold for defining hypogonadism varies across guidelines, and the relationship between biochemical levels and symptoms is not always linear. This demands individualized judgment rather than rigid adherence to numerical cutoffs.
Conclusion
Erectile dysfunction is a multifactorial condition with profound personal and clinical consequences. Testosterone plays a critical role in maintaining sexual desire, erectile physiology, and responsiveness to pharmacotherapy. While not every case of ED is androgen-dependent, a substantial subset of men—particularly those with hypogonadism—benefit significantly from testosterone replacement.
Evidence supports the use of testosterone therapy both as monotherapy in hypogonadal men and as an adjunct to PDE5 inhibitors in refractory cases. Screening for hypogonadism in men with ED, especially those unresponsive to PDE5Is, should therefore be standard practice.
By recognizing the interplay between testosterone and erectile physiology, clinicians can provide more effective, individualized care. Ultimately, the integration of hormone therapy with modern pharmacology exemplifies a broader principle in medicine: optimal outcomes often emerge from addressing both the underlying biology and the symptomatic expression of disease.
FAQ
1. Should all men with erectile dysfunction receive testosterone therapy?
No. Testosterone therapy is indicated primarily for men with documented hypogonadism and symptoms such as low libido or ED. Men with normal testosterone levels typically do not benefit from supplementation.
2. Why do some men fail to respond to sildenafil?
Failure may reflect inadequate testosterone levels, severe vascular disease, neuropathy, or psychological factors. In hypogonadal men, restoring testosterone often enhances responsiveness to PDE5 inhibitors.
3. Is testosterone therapy safe in the long term?
When properly monitored, testosterone therapy is generally safe. Regular assessments of hematocrit, PSA, and cardiovascular health are essential. Current data do not support an increased risk of prostate cancer, but long-term studies are ongoing.


