Introduction
Pulmonary hypertension (PH) remains one of the most formidable challenges in modern cardiology. Defined by abnormally elevated pulmonary arterial pressures, it is both a disease in itself and a complication of diverse cardiovascular and respiratory conditions. Patients with PH experience progressive dyspnea, exercise intolerance, and right heart failure. Prognosis, without targeted therapy, is often dismal. While primary pulmonary arterial hypertension has attracted significant research interest, secondary pulmonary hypertension, arising from left heart disease, chronic lung pathology, or thromboembolic disorders, constitutes the majority of cases encountered in practice.
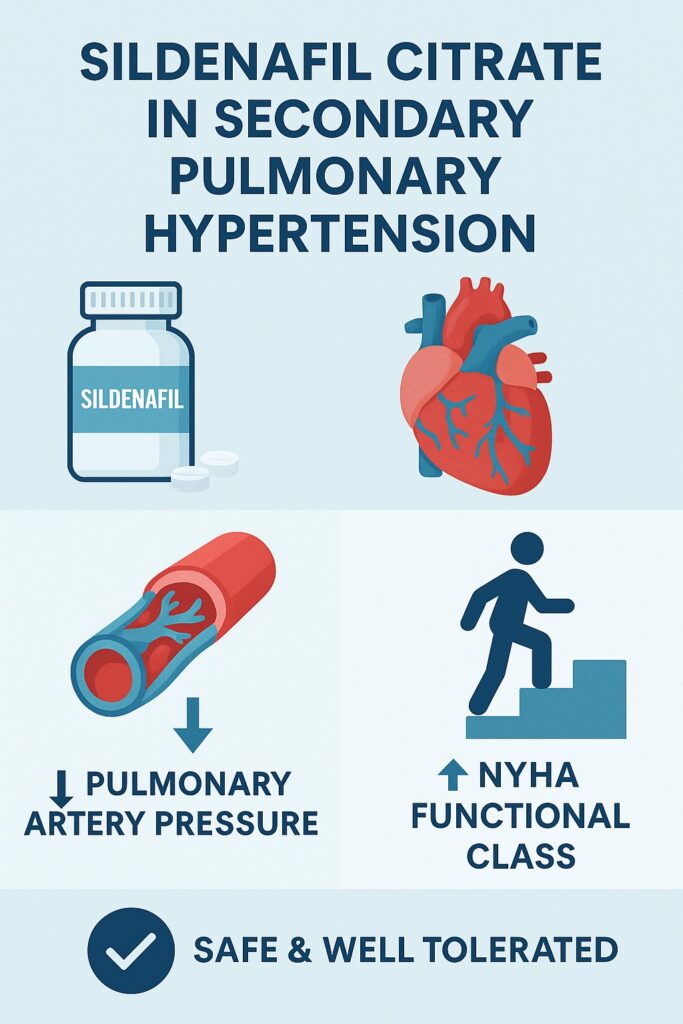
In recent years, pharmacological strategies have sought to repurpose vasodilators originally designed for other indications. Among these, sildenafil citrate, a phosphodiesterase type 5 (PDE5) inhibitor best known for treating erectile dysfunction, has emerged as a promising agent. By augmenting the nitric oxide (NO)–cGMP pathway, sildenafil induces selective pulmonary vasodilation and improves right ventricular afterload. Yet, the translation of these molecular effects into clinical benefits for secondary PH has been less consistently documented.
A 2014 study published in The Egyptian Heart Journal addressed this knowledge gap through a randomized, placebo-controlled trial assessing the short-term efficacy and safety of sildenafil in patients with symptomatic secondary PH. The findings, while modest in duration, shed important light on the therapeutic promise and limitations of PDE5 inhibition in this challenging population.
Pathophysiology of Secondary Pulmonary Hypertension
Secondary pulmonary hypertension is not a uniform entity. Its pathogenesis varies depending on the underlying disease. In patients with left heart disease, backward transmission of elevated filling pressures leads to pulmonary venous hypertension, endothelial dysfunction, and subsequent arteriolar remodeling. In chronic lung disease such as COPD or interstitial fibrosis, hypoxic vasoconstriction and vascular remodeling predominate. In chronic thromboembolic pulmonary hypertension (CTEPH), unresolved emboli create both mechanical obstruction and secondary vascular changes.
Despite these differences, a final common pathway emerges: endothelial dysfunction with impaired nitric oxide signaling, increased endothelin activity, and structural remodeling of pulmonary vessels. The result is elevated pulmonary vascular resistance, right ventricular hypertrophy, and eventual right heart failure.
Conventional therapy—diuretics, oxygen supplementation, and anticoagulation—addresses symptoms but rarely alters disease trajectory. Hence, the appeal of agents such as sildenafil that target the molecular pathways underpinning pulmonary vascular tone.
Pharmacological Rationale for Sildenafil in Pulmonary Hypertension
Sildenafil is a selective PDE5 inhibitor, preventing degradation of cyclic guanosine monophosphate (cGMP). By prolonging cGMP activity in pulmonary vascular smooth muscle, sildenafil enhances nitric oxide–mediated vasodilation. PDE5 is expressed abundantly in pulmonary vasculature, making this pathway a rational therapeutic target.
Preclinical studies demonstrated that sildenafil reduces pulmonary artery pressure, improves right ventricular function, and limits vascular remodeling. Clinical investigations in primary pulmonary arterial hypertension (PAH) confirmed improvements in 6-minute walk distance, hemodynamics, and functional class. These successes encouraged exploration of sildenafil in secondary PH, where endothelial dysfunction and vasoconstriction also play prominent roles.
However, skepticism persisted. Would vasodilation exacerbate pulmonary congestion in left heart disease? Would structural vascular changes in chronic lung disease blunt its efficacy? The Egyptian study provided valuable real-world insight into these questions.
Study Design and Patient Population
The 2014 trial enrolled 40 patients with symptomatic secondary PH of diverse etiologies: rheumatic or prosthetic valve disease, COPD, chronic thromboembolism, interstitial lung fibrosis, and dilated cardiomyopathy. All patients had documented elevated pulmonary artery systolic pressures (PASP) by echocardiography and significant functional limitation (NYHA class II–IV).
Participants were randomized into two groups:
- Treatment arm: received sildenafil citrate for six weeks.
- Control arm: received placebo alongside standard medical care.
Key endpoints included changes in pulmonary artery systolic pressure, left ventricular ejection fraction (LVEF), and NYHA functional class. Safety was also closely monitored. This short-term design offered a focused lens on the immediate physiological and symptomatic impact of sildenafil in secondary PH.
Results: Hemodynamic and Functional Outcomes
The findings were encouraging. Patients treated with sildenafil demonstrated a significant reduction in PASP compared to the placebo group. This effect was consistent across etiologies, suggesting broad applicability. Importantly, the vasodilatory effect did not precipitate pulmonary edema or worsen left heart filling pressures, alleviating a key concern in post-capillary PH.
Functional outcomes mirrored hemodynamic improvements. Approximately 75% of sildenafil patients improved by at least one NYHA functional class, compared to only 20% of controls. This translated into meaningful gains in exercise tolerance and quality of life.
Left ventricular ejection fraction showed a trend toward improvement in the sildenafil group, though differences did not reach statistical significance. Given the study’s short duration and small sample, this was unsurprising. Nonetheless, even marginal gains in LVEF may be clinically relevant when considered alongside reduced pulmonary pressures.
Safety and Tolerability
Sildenafil was generally well tolerated. Reported side effects were mild and transient, including headache, flushing, and nausea. No patients discontinued therapy due to adverse events. Crucially, no episodes of significant hypotension, arrhythmia, or pulmonary edema were observed, underscoring the relative safety of PDE5 inhibition even in patients with advanced cardiac and pulmonary comorbidities.
This tolerability profile aligns with broader clinical experience in both erectile dysfunction and PAH populations. For secondary PH patients, many of whom are frail and heavily medicated, such reassurance is vital.
Mechanistic Interpretations
The benefits observed in this trial likely reflect sildenafil’s ability to restore NO–cGMP signaling, reduce pulmonary vascular resistance, and enhance right ventricular–pulmonary arterial coupling. By lowering afterload, sildenafil may improve right ventricular stroke volume, indirectly supporting left ventricular filling and cardiac output.
Additionally, sildenafil’s antioxidant and anti-proliferative effects on vascular smooth muscle may contribute to early remodeling benefits, although such structural effects would require longer treatment to manifest clearly.
The absence of adverse pulmonary congestion suggests that, at least in the short term, vasodilation did not exacerbate hydrostatic pressures in patients with left heart disease—a finding of considerable practical significance.
Clinical Implications
The study offers several important lessons for clinicians:
- Efficacy across etiologies: Sildenafil reduced pulmonary pressures and improved symptoms regardless of whether PH stemmed from valvular disease, COPD, thromboembolic disease, or cardiomyopathy.
- Rapid symptomatic relief: Significant improvements were observed within six weeks, a meaningful timeframe for patients struggling with daily functional limitations.
- Safety reassurance: The absence of serious adverse effects supports cautious but confident use of sildenafil in carefully selected patients with secondary PH.
Nevertheless, limitations must temper enthusiasm. The study’s small size and short duration preclude definitive conclusions about long-term survival, remodeling, or disease progression. Moreover, echocardiographic PASP estimation, while practical, is less precise than right heart catheterization.
Broader Context: Where Does Sildenafil Fit?
In the therapeutic hierarchy of secondary PH, sildenafil occupies an ambiguous but increasingly intriguing position. Current international guidelines remain conservative, generally discouraging routine PDE5 inhibitor use outside primary PAH or CTEPH pending stronger evidence. However, growing data—including this Egyptian study—suggest a role for sildenafil as adjunctive therapy in symptomatic secondary PH unresponsive to conventional measures.
Future trials must clarify patient selection criteria. Those with predominantly reactive vasoconstrictive components may benefit most, while patients with fixed structural remodeling may experience limited gains. Similarly, in post-capillary PH due to left heart disease, careful monitoring remains essential to avoid exacerbating congestion.
Conclusion
The short-term trial of sildenafil citrate in secondary pulmonary hypertension provides compelling evidence that this well-known PDE5 inhibitor confers measurable hemodynamic and symptomatic benefits across diverse etiologies of PH. By lowering pulmonary pressures and improving functional status, sildenafil enhances quality of life while maintaining a favorable safety profile.
While larger, longer trials are essential to establish its impact on survival and remodeling, the study highlights sildenafil’s potential as a valuable adjunct in the multidisciplinary management of secondary PH. For patients facing daily limitations from breathlessness and fatigue, even modest short-term gains can be life-changing.
FAQ
1. Can sildenafil be used routinely for all patients with secondary pulmonary hypertension?
Not yet. Current evidence supports its potential benefits, but larger trials are needed. At present, its use should be individualized and closely monitored.
2. How quickly does sildenafil improve symptoms in pulmonary hypertension?
In the study, improvements in pulmonary pressure and NYHA functional class were evident within six weeks, indicating relatively rapid benefit.
3. Is sildenafil safe in patients with left heart disease–related pulmonary hypertension?
Short-term data suggest it is safe and effective without worsening congestion, but careful patient selection and monitoring are essential.


