Introduction
Few challenges in perinatal medicine are as persistent and clinically relevant as intrauterine growth restriction (IUGR). Affecting up to 15% of pregnancies worldwide, IUGR is more than a statistical burden: it is a powerful predictor of perinatal mortality, neonatal morbidity, and the risk of chronic diseases in adulthood. Babies who fail to grow adequately in the womb face lifelong disadvantages, from metabolic syndrome to impaired cognitive development.
At the heart of IUGR lies a recurring villain—insufficient uteroplacental blood flow and nutrient transfer. Despite decades of research, truly effective interventions remain scarce. Dietary adjustments, bed rest, and supplemental oxygen have historically been tried with minimal success. Recently, however, pharmacological strategies targeting uteroplacental perfusion have gained attention, and sildenafil citrate—a drug more famously marketed for erectile dysfunction—has emerged as an unlikely but promising candidate.
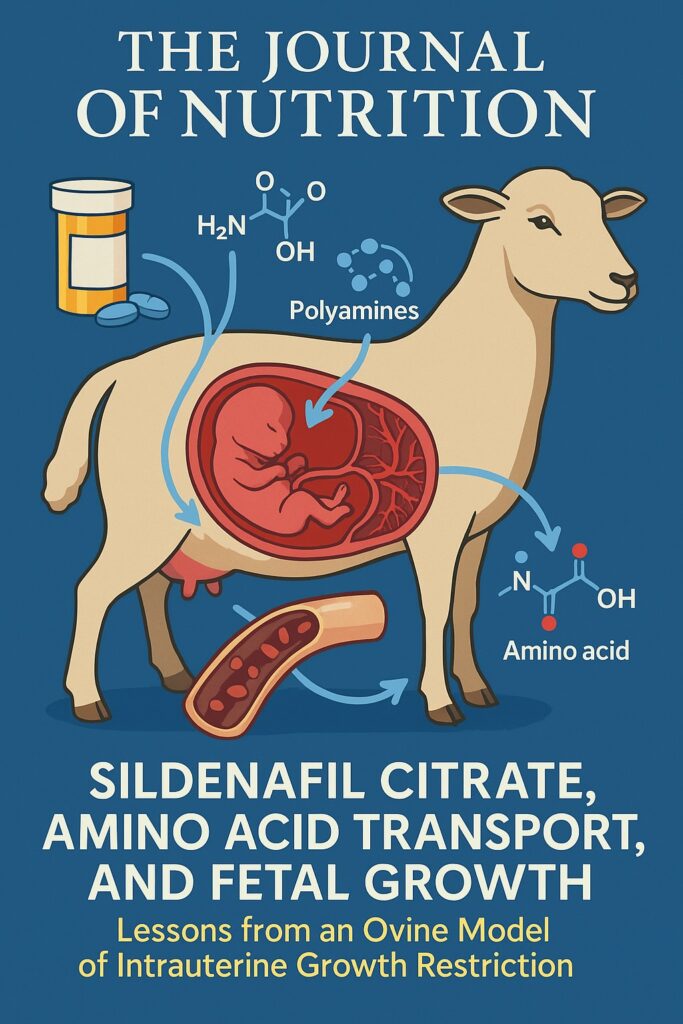
The study under discussion used an ovine model to explore how maternal administration of sildenafil citrate influences fetal growth, amino acid transport, and conceptus development. Its findings provide both mechanistic insights and tantalizing therapeutic possibilities. This article dissects the experimental design, interprets the results, and places them within the broader context of maternal-fetal medicine.
The Biology of Intrauterine Growth Restriction
IUGR arises when a fetus fails to achieve its genetic growth potential, usually due to placental insufficiency. While genetics and infections play occasional roles, the overwhelming majority of cases result from inadequate nutrient and oxygen transfer across the placenta. The placenta, often underappreciated outside of obstetrics, serves as the gatekeeper of fetal nutrition, regulating glucose, amino acids, lipids, and growth factors.
Restricted uteroplacental blood flow is the most consistent finding in IUGR. Reduced perfusion limits maternal-fetal exchange, starving the fetus of essential substrates. Notably, amino acid transport is profoundly impaired in these pregnancies. Given that amino acids not only build proteins but also act as signaling molecules, neurotransmitter precursors, and regulators of angiogenesis, their shortage has catastrophic consequences for fetal growth and organ development.
The sheep, or ovine model, is particularly well-suited to study IUGR. Its placentation closely resembles that of humans, and interventions can be performed with high translational relevance. Nutrient restriction in pregnant ewes reliably induces fetal growth restriction, reproducing key features of the human condition. Against this backdrop, sildenafil citrate was introduced as a potential rescue strategy.
Sildenafil Citrate: From Erectile Dysfunction to Uteroplacental Therapy
Sildenafil citrate’s claim to fame lies in the inhibition of phosphodiesterase type 5 (PDE5). By preventing PDE5-mediated degradation of cyclic guanosine monophosphate (cGMP), sildenafil amplifies nitric oxide (NO)-driven vasodilation. In erectile tissue, this results in improved blood inflow. But the pharmacological principle is generalizable: wherever PDE5 is expressed and NO is available, sildenafil may enhance vascular relaxation.
Evidence from myometrial and uterine arteries suggested that sildenafil augments vasodilation in pregnant women, particularly those with IUGR. In animal models, the drug improved uterine perfusion and reduced systemic vascular resistance. Translating these effects into the maternal-fetal unit raised the hypothesis: could sildenafil restore nutrient transfer and thereby stimulate fetal growth?
Unlike glucose, which can diffuse passively, amino acids depend heavily on active transport across placental membranes. NO and cGMP signaling regulate angiogenesis and transporter activity, linking vascular tone directly to nutrient delivery. By this reasoning, sildenafil could act as more than a hemodynamic agent; it could reshape the biochemical landscape of the conceptus.
Experimental Design: The Ovine Model of Nutrient Restriction
The investigators designed a 2 × 3 factorial experiment. Sixty Suffolk ewes were divided into groups based on diet (adequate feeding at 100% NRC requirements versus nutrient restriction at 50%) and sildenafil citrate dosage (0, 75, or 150 mg/day). Treatment spanned days 28–115 of gestation, a period encompassing placental maturation and rapid fetal growth.
Sildenafil was administered subcutaneously three times daily, mimicking sustained exposure. At day 115, ewes were humanely sacrificed, and samples were collected: maternal blood, placental tissues, fetal fluids (amniotic and allantoic), and fetal serum from the umbilical vein. Fetal weights and organ measurements were recorded. Amino acids and polyamines were quantified using high-performance liquid chromatography, while metabolic intermediates such as glucose, lactate, and urea were also assessed.
This meticulous design allowed investigators to disentangle the independent and interactive effects of diet and sildenafil on fetal growth and biochemical profiles. Importantly, only singleton pregnancies were analyzed, avoiding the confounding impact of litter size.
Maternal and Placental Observations
As expected, nutrient restriction profoundly impacted maternal physiology. Restricted ewes lost significantly more body weight, had lower body condition scores, and exhibited smaller liver and muscle masses compared to adequately fed controls. Interestingly, sildenafil had minimal direct effects on maternal weight or organ size. Its action seemed confined to nutrient trafficking rather than maternal energy balance.
Placental parameters such as weight and number of placentomes were not significantly altered by sildenafil treatment. This suggests that the drug did not enlarge the placenta itself but may have improved its functional capacity. This distinction is important: enhancing placental nutrient transport can be as effective as increasing placental mass.
In other words, sildenafil did not remodel the maternal body or gross placental morphology. Instead, its magic appeared to operate at the level of nutrient flow and molecular exchange.
Effects on Fetal Growth and Organ Development
The primary outcome—fetal weight at day 115—showed compelling results. Fetuses from nutrient-restricted ewes weighed significantly less than those from adequately fed mothers, validating the IUGR model. Yet sildenafil citrate reversed much of this deficit.
- At 75 mg/day, fetal weights increased modestly but significantly.
- At 150 mg/day, fetal weights rose more substantially, even surpassing untreated adequately fed controls in some comparisons.
Importantly, this effect was observed regardless of maternal diet, meaning sildenafil enhanced fetal growth in both nutrient-restricted and adequately nourished pregnancies.
When fetal organ weights were analyzed relative to body weight, most proportions remained unchanged, indicating proportional growth rather than selective organomegaly. Exceptions included subtle increases in the left ventricle and pancreas under certain conditions. This is clinically relevant: disproportionate organ growth can signal pathological adaptation, but proportional catch-up growth suggests healthier development.
Amino Acid Availability: The Central Mechanism
Perhaps the most striking findings were biochemical. Nutrient restriction reduced amino acid concentrations across maternal, fetal, and placental compartments. This shortage was precisely what one would expect in IUGR.
Sildenafil citrate, however, dose-dependently increased amino acid levels in fetal serum, amniotic fluid, and allantoic fluid. The effect was robust: nearly all amino acids—arginine, glutamine, glycine, serine, valine, and more—rose significantly in treated animals. Total amino acid concentrations in fetal serum reached levels far exceeding untreated controls.
The fetal:maternal serum amino acid ratios also improved with sildenafil, indicating enhanced placental transfer efficiency rather than mere maternal spillover. This ratio is a critical index of placental transporter function, and its improvement directly links sildenafil’s vascular effects to nutrient supply.
In short, sildenafil transformed the biochemical milieu of the fetus from scarcity to abundance, giving developing tissues the raw materials required for growth.
Polyamines and Their Role in Placental Growth
Beyond amino acids, the study measured polyamines—small polycationic molecules such as spermidine and spermine, synthesized from amino acid precursors. Polyamines regulate angiogenesis, DNA synthesis, and cell proliferation. They are indispensable for placental and fetal development.
Nutrient restriction reduced polyamine concentrations in all compartments, but sildenafil treatment reversed this deficit. Elevated polyamine levels in fetal blood and fluids likely supported enhanced cellular proliferation and vascular development. By boosting both amino acid precursors and polyamine synthesis, sildenafil created a biochemical cascade favoring fetal growth.
This finding is particularly important because polyamines have been directly linked to placental angiogenesis. Improved angiogenesis translates into better long-term nutrient delivery, reinforcing sildenafil’s therapeutic potential.
Metabolic Intermediates and Lactate Dynamics
The study also tracked metabolites like glucose, lactate, urea, and ammonia. Surprisingly, sildenafil’s effects here were more nuanced. Glucose concentrations were not significantly altered, reflecting its different transport mechanisms. Lactate, however, rose consistently with sildenafil treatment.
This rise in lactate is not necessarily harmful. Lactate serves as an energy substrate for the fetus and may indicate enhanced glycolytic flux. The observed increases likely reflect better substrate availability and utilization, consistent with the growth-promoting effects of the drug.
Taken together, the metabolic data confirm that sildenafil selectively targeted amino acid and polyamine pathways rather than broadly altering all nutrients.
Translational Implications for Human Medicine
The obvious question is whether these findings translate to human pregnancies complicated by IUGR. Several points support cautious optimism:
- Mechanistic plausibility: PDE5 inhibition enhances uteroplacental blood flow and transporter function, mechanisms conserved across species.
- Biochemical parallels: Amino acid deficiencies are central in human IUGR, just as in sheep.
- Precedent: Early human studies showed sildenafil-induced vasodilation in myometrial arteries from IUGR pregnancies.
However, clinical translation requires caution. Dosing regimens, pharmacokinetics, and safety profiles differ between sheep and humans. Moreover, the human placenta has unique transporter dynamics. Large-scale randomized controlled trials would be required before sildenafil could be recommended clinically.
Still, the ovine findings provide a compelling rationale for further exploration. If safe, sildenafil could represent the first pharmacological intervention to directly enhance fetal nutrient availability, shifting the paradigm of IUGR management.
Limitations and Future Directions
Like all studies, this work has limitations. The ovine model, while valuable, is not identical to human pregnancy. The doses of sildenafil used were high and may not correspond directly to human therapeutic ranges. Additionally, the study did not measure uterine blood flow directly, leaving the exact hemodynamic mechanism inferred rather than proven.
Future research should:
- Assess long-term offspring outcomes, including metabolic health and organ function.
- Explore optimal timing and duration of therapy—whether early versus late gestation matters.
- Investigate potential side effects, particularly on maternal cardiovascular function.
- Test combinatory approaches with amino acid supplementation to determine additive benefits.
Such studies could pave the way for clinical trials in women with pregnancies at risk of IUGR.
Conclusion
This study elegantly demonstrated that sildenafil citrate enhances fetal growth in sheep by increasing amino acid and polyamine availability, independent of maternal diet. By improving the efficiency of nutrient transfer across the placenta, sildenafil provided the fetus with the essential building blocks of growth, resulting in larger and healthier offspring.
The implications extend beyond veterinary science. For human obstetrics, where IUGR remains a frustratingly unsolved problem, these findings offer a glimmer of therapeutic hope. A drug once confined to the realm of male sexual health may yet find a second life as a guardian of fetal well-being. The journey from ovine models to delivery rooms is not trivial, but it is one worth undertaking.
FAQ
1. How does sildenafil improve fetal growth?
By inhibiting PDE5, sildenafil enhances uteroplacental blood flow and nutrient transfer. This increases amino acid and polyamine availability in the fetus, which are essential for growth and development.
2. Could sildenafil be used in pregnant women with IUGR?
The ovine data are promising, but human trials are needed. Early studies suggest potential benefits, but safety and efficacy must be rigorously tested before clinical adoption.
3. Why focus on amino acids rather than glucose?
Although glucose is important, amino acids are critical for protein synthesis, cell signaling, and angiogenesis. In IUGR, amino acid transport is especially impaired, making it a key target for intervention.


