Erectile dysfunction (ED) remains one of the most distressing complications for men with type 2 diabetes mellitus (T2DM). While pharmacological treatments such as phosphodiesterase-5 inhibitors (PDE5i) are widely prescribed, they do not always yield satisfactory results, nor are they appropriate for every patient. In recent years, attention has turned toward non-medical and non-invasive interventions. These strategies, ranging from lifestyle modification to the use of assistive devices, not only target erectile health but also enhance overall metabolic control and psychological well-being.
This article explores the scope of evidence regarding non-medical interventions for ED in men with T2DM, drawing upon the latest scoping review literature while providing a structured and clinically relevant narrative.
Understanding the Burden of ED in Type 2 Diabetes
Erectile dysfunction is more than an inconvenience; it is a sentinel marker of systemic vascular damage. Men with T2DM are nearly three times more likely to develop ED compared to their non-diabetic peers. Chronic hyperglycemia causes endothelial dysfunction, small artery impairment, and neuropathy, all of which contribute to impaired penile blood flow and erection.
Additionally, many men with T2DM experience hypogonadotropic hypogonadism—a reduction in testosterone levels due to impaired hypothalamic and pituitary signaling. The combination of vascular and hormonal disruption creates an environment ripe for ED development, often within just five years of diabetes diagnosis.
Psychological sequelae cannot be underestimated. ED is strongly linked with depression, marital tension, and reduced quality of life. For many men, sexual health is integral to identity and intimate relationships; thus, failure to address ED perpetuates frustration, anxiety, and emotional withdrawal.
Why Look Beyond Medication?
The widespread use of PDE5 inhibitors has provided relief to countless men. However, there are important limitations:
- A proportion of patients are non-responders to PDE5i, often due to severe vascular impairment.
- Side effects such as headache, flushing, and visual disturbances may limit tolerability.
- Certain comorbidities and concomitant medications make PDE5i unsafe or less effective.
- Many men prefer to avoid invasive treatments, such as injections or implants.
Therefore, non-medical and non-invasive strategies are more than alternatives—they are essential components of a holistic approach to diabetic sexual health.
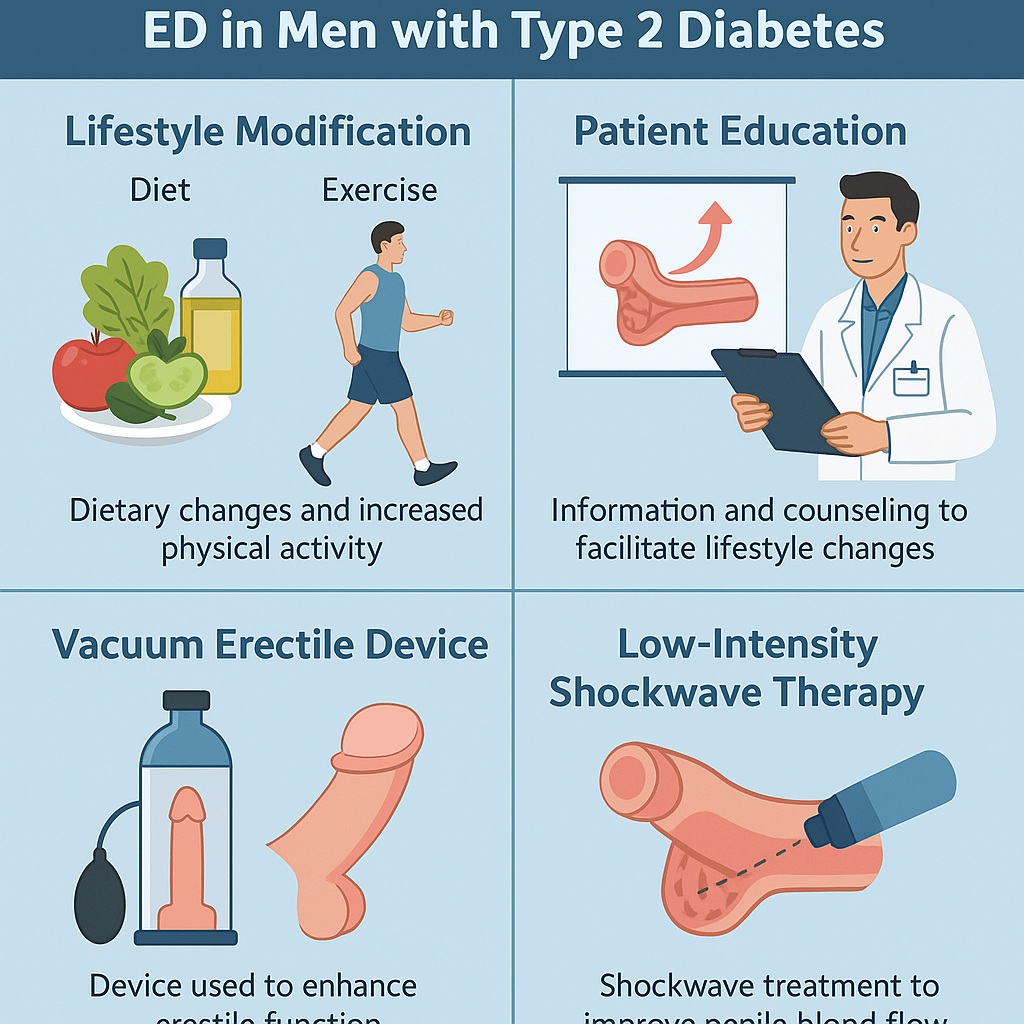
The Power of Patient Education
Patient education consistently emerges as the cornerstone of successful non-medical management. Studies emphasize that informed patients are more likely to adopt lifestyle changes, adhere to treatment plans, and proactively manage their health.
Education in this context extends beyond generic advice. Effective programs involve multidisciplinary teams—including dieticians, physical therapists, pharmacists, nurses, and psychologists—who guide men in self-monitoring, dietary adjustments, physical activity, and stress management.
For instance, structured education models such as the MEDIC program (Multidisciplinary Education in Diabetes and Intervention for Cardiac Risk Reduction) have demonstrated measurable improvements in erectile function. By addressing comorbidities like hypertension, dyslipidemia, and tobacco use, these interventions indirectly enhance erectile capacity.
The lesson is clear: knowledge is not a passive asset but an active therapeutic tool. Without patient education, lifestyle interventions are far less likely to succeed.
Lifestyle Modification: Diet and Exercise as First-Line Therapy
Among the reviewed evidence, lifestyle modification stands out as the most consistently effective intervention. This includes both dietary adjustment and physical activity.
Dietary Interventions
A Mediterranean-style diet, characterized by high consumption of fruits, vegetables, whole grains, legumes, nuts, and olive oil, along with limited red meat and saturated fats, has been repeatedly associated with improved erectile outcomes.
In randomized trials, men adhering to such diets not only achieved better glycemic control but also demonstrated significantly higher scores on the International Index of Erectile Function (IIEF). The mechanisms are multifactorial: improved endothelial function, reduced oxidative stress, lower systemic inflammation, and favorable lipid profiles all converge to restore vascular health essential for erection.
Low-calorie diets have also shown promise. Even modest weight reduction—around 5–10% of body weight—has been correlated with meaningful improvements in erectile function. The act of losing weight reduces insulin resistance, lowers blood pressure, and boosts testosterone levels.
Physical Activity
Exercise is equally indispensable. Regular aerobic activity such as brisk walking, swimming, or cycling enhances cardiovascular health and increases nitric oxide bioavailability, which is central to penile vasodilation. Strength training contributes by improving insulin sensitivity and promoting muscle mass, further aiding metabolic stability.
Studies suggest that men who engage in structured physical activity are up to 40% less likely to experience ED compared to sedentary peers. Importantly, the threshold for benefit is attainable: 150 minutes of moderate-intensity exercise per week, or simply a daily 30-minute walk, can yield significant results.
Assistive Devices: Vacuum Erectile Device (VED)
For men who require more immediate mechanical assistance, the vacuum erectile device provides a safe and non-invasive option. By creating negative pressure around the penis, VED facilitates blood flow into the corpora cavernosa, inducing an erection that can be maintained with a constriction ring.
Clinical studies report satisfaction rates of up to 85%. Although some men experience discomfort, numbness, or bruising, these are generally minor and reversible with proper instruction and moderation.
VED is particularly valuable for men who either cannot tolerate PDE5i or wish to avoid pharmacological interventions altogether. It is also an effective adjunct for those with partial PDE5i response, enhancing rigidity and confidence.
Low-Intensity Extracorporeal Shockwave Therapy (Li-ESWT)
One of the most intriguing developments in non-invasive ED treatment is low-intensity extracorporeal shockwave therapy. This approach involves applying focused shockwaves to the penile shaft and crura, stimulating neovascularization and improving penile blood flow.
Although the therapy remains under investigation, multiple trials in men with diabetes-related ED have shown improvements in IIEF scores, particularly when combined with other interventions such as pelvic floor exercises or PDE5i.
Importantly, Li-ESWT is painless, requires no anesthesia, and has not been associated with significant adverse events. However, it should be delivered by trained professionals, and long-term efficacy still requires confirmation through larger, multicenter trials.
Integration of Multimodal Approaches
A recurring theme in the literature is that no single intervention guarantees success for every patient. Instead, multimodal strategies appear most effective. For example, a man with T2DM and ED may benefit from:
- A Mediterranean diet and structured exercise to improve metabolic health.
- A patient education program to reinforce adherence and provide psychological support.
- A VED as a practical aid for sexual activity.
- Li-ESWT as a specialist-administered adjunct therapy.
The combination of these elements addresses not only the symptom of ED but also the underlying vascular and metabolic dysfunctions driving it.
The Importance of Early Intervention
Timing is critical. Men who adopt lifestyle modifications soon after diabetes diagnosis are far more likely to preserve erectile function than those who delay until irreversible vascular damage has occurred.
Unfortunately, screening for ED in men with T2DM is inconsistent, and many only present once their relationships and self-esteem are severely affected. Clinicians should therefore view ED as a clinical warning sign, prompting both metabolic optimization and targeted sexual health interventions.
Early identification and proactive management can prevent years of frustration, improve quality of life, and reduce the burden of diabetic complications.
Limitations of Current Evidence
While the available studies are promising, several limitations must be acknowledged:
- Most research originates from high-income countries; data from low-resource settings are lacking.
- Sample sizes are often modest, limiting generalizability.
- Long-term follow-up is scarce, particularly for interventions like Li-ESWT.
- Gray literature and unpublished data were excluded, potentially omitting relevant findings.
Nonetheless, the consistency of positive outcomes across diverse interventions lends credibility to the overall conclusions.
Clinical Implications
For healthcare professionals, the implications are straightforward yet profound:
- Do not rely solely on pharmacological treatments.
- Incorporate patient education as a structured component of diabetes management.
- Recommend Mediterranean diet and regular exercise as first-line therapy for diabetic men with ED.
- Consider VED or Li-ESWT as adjunctive measures when lifestyle interventions alone are insufficient.
- Screen routinely for ED in men with T2DM, even if they do not explicitly complain of sexual dysfunction.
Such an integrated approach aligns sexual health with holistic diabetes care, ensuring men achieve both improved metabolic control and enhanced quality of life.
Conclusion
Erectile dysfunction in men with type 2 diabetes is not merely a private concern but a public health issue that reflects systemic vascular health. While pharmacological therapies have their place, non-medical and non-invasive interventions provide equally important, and sometimes superior, avenues for management.
Dietary modification, physical activity, patient education, assistive devices, and emerging energy-based therapies collectively represent a powerful arsenal against T2DM-associated ED. More importantly, they empower men to take control of their health in a sustainable, non-invasive manner.
By prioritizing early intervention, multidisciplinary education, and lifestyle modification, clinicians can help men with T2DM not only restore erectile function but also reclaim vitality, confidence, and well-being.
FAQ
1. Can lifestyle changes alone reverse erectile dysfunction in men with type 2 diabetes?
Yes—particularly when adopted early. Weight loss, improved diet, and regular exercise can significantly enhance erectile function by improving vascular and hormonal balance. However, results vary, and some men may require additional interventions such as VED or PDE5 inhibitors.
2. Is vacuum erectile device therapy safe for diabetic men?
Generally, yes. VED is considered safe and effective when used correctly. Minor side effects such as discomfort, bruising, or numbness may occur but are usually manageable. Medical supervision is recommended to ensure proper use.
3. How effective is shockwave therapy for diabetes-related ED?
Low-intensity extracorporeal shockwave therapy shows promising results in stimulating penile blood flow and improving erectile function. However, it remains an emerging treatment, and larger long-term studies are needed to establish its role.


