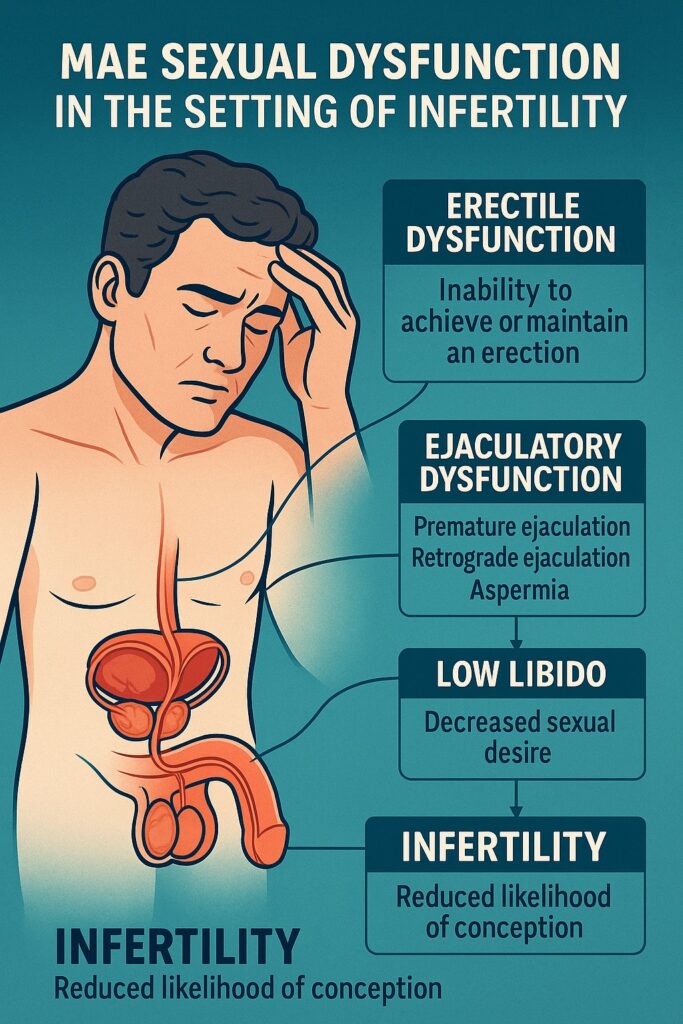
Infertility is not merely a biological limitation; it is an emotional storm that reshapes intimate partnerships and burdens individual identity. For male patients, sexual dysfunction often represents both a cause and a consequence of infertility. Erectile difficulties, ejaculatory disorders, and diminished libido may be the first indicators of deeper endocrine, vascular, or psychological disturbances. The modern clinician must therefore treat not only the seminal fluid but also the subtle interplay of health, confidence, and sexual vitality.
This article synthesizes current knowledge on the evaluation and management of male sexual dysfunction when infertility is the presenting complaint. Drawing on the latest committee guidelines and contemporary clinical practice, it aims to equip the clinician with both the science and the art necessary to navigate this delicate terrain.
Erectile Dysfunction in Infertile Men
Understanding the Clinical Burden
Erectile dysfunction (ED) is defined as the persistent inability to achieve or maintain an erection sufficient for satisfactory sexual activity. While definitions are easy to recite, the human impact is less readily summarized. In men undergoing infertility evaluation, ED is more common than in the general population. Estimates suggest that between 18% and 89% of infertile men experience ED, with prevalence far exceeding that of fertile controls.
Why such a staggering range? The variability reflects the complex biology of erection, but also the sociocultural, psychological, and relational stressors amplified by the experience of infertility. A man who once performed confidently in the bedroom may falter under the pressure of scheduled intercourse, sperm collection, or repeated failed cycles.
Organic Versus Psychogenic Factors
Clinically, ED in infertile men can be broadly categorized into psychogenic and organic origins:
- Psychogenic ED often appears situational. The patient may achieve erections during masturbation or upon waking but struggle in intercourse when conception is the goal. It is the cruel paradox of performance anxiety: the harder one tries, the less one succeeds.
- Organic ED reflects vascular insufficiency, neuropathy, or endocrine dysfunction. Age, diabetes, hypertension, and cardiovascular disease frequently play the starring roles. Unlike psychogenic ED, organic dysfunction persists across all contexts.
The challenge for clinicians lies in distinguishing between the two, while remembering they often overlap. Indeed, a man with vascular disease may still feel compounded performance anxiety, creating a cycle of dysfunction that resists single-label classification.
Diagnostic Evaluation
History-taking remains the cornerstone. A meticulous inquiry into comorbidities, surgeries, smoking habits, medications, and relationship dynamics uncovers both obvious and hidden contributors. Standardized questionnaires such as the International Index of Erectile Function (IIEF) or the Sexual Health Inventory for Men lend structure and allow baseline severity to be documented.
Physical examination should not be neglected. Blood pressure measurement, BMI calculation, and signs of hypogonadism may reveal systemic contributors. Morning serum testosterone, glucose levels, HbA1c, and lipid profile round out the initial laboratory evaluation. For ambiguous cases, penile Doppler ultrasonography or nocturnal penile tumescence testing can help distinguish organic from psychogenic pathology.
Management Pathways
Treatment must begin with reassurance: erectile dysfunction is not a referendum on masculinity or love. From there, management proceeds in layers:
- Lifestyle optimization: weight reduction, exercise, smoking cessation, and dietary changes.
- Pharmacotherapy: Phosphodiesterase type-5 inhibitors (PDE5i) such as sildenafil, tadalafil, and vardenafil remain first-line agents. Patients must be counseled on risks, contraindications (notably nitrates), and potential side effects ranging from headaches to visual changes.
- Psychological support: counseling, sex therapy, or referral to mental health professionals may transform the trajectory of psychogenic ED.
- Advanced interventions: intracavernosal injections or penile prosthesis implantation are options when conservative strategies fail.
For infertile men, timely ED management carries additional urgency. An untreated erection problem may not only sabotage natural conception but also complicate assisted reproductive procedures requiring on-demand specimen collection.
Ejaculatory Dysfunction and Fertility Potential
Defining the Spectrum
Ejaculation is the biological endpoint of male sexual function, but when disrupted, it can derail fertility prospects entirely. Ejaculatory dysfunction encompasses a spectrum ranging from aspermia (no ejaculation) to retrograde ejaculation (sperm redirected into the bladder) to premature ejaculation (PE), where ejaculation occurs too quickly to permit effective conception.
Each variant has unique implications for fertility: aspermia and retrograde ejaculation prevent semen deposition, while PE may render intercourse unsuccessful before ovum exposure.
Etiological Pathways
Causes of ejaculatory dysfunction are diverse:
- Neurological injury from spinal cord trauma or pelvic surgery.
- Retrograde ejaculation after bladder neck or prostate surgery, or due to medications such as alpha-blockers.
- Diabetes mellitus, notorious for neuropathic disruption of emission and expulsion phases.
- Psychological contributors, which often amplify premature ejaculation.
Clinicians must also be aware of rare structural anomalies such as ejaculatory duct obstruction.
Diagnostic and Therapeutic Approaches
Diagnosis requires clear history-taking, supplemented by post-ejaculatory urine analysis in suspected retrograde cases. When emission fails altogether, as after retroperitoneal lymph node dissection, the prognosis is poor and sperm retrieval becomes the only option.
Management strategies vary:
- Retrograde ejaculation may respond to discontinuation of causative drugs or administration of alpha-agonists or tricyclic antidepressants like imipramine. When unsuccessful, sperm harvested from post-ejaculatory urine can be used for intrauterine insemination (IUI) or IVF.
- Premature ejaculation benefits from multimodal therapy: behavioral methods, topical anesthetics, and pharmacological agents such as selective serotonin reuptake inhibitors (SSRIs). Crucially, sexual therapy that includes the partner often improves not only latency but also relationship satisfaction.
- Aspermia due to neurologic or structural causes may require vibratory stimulation, electroejaculation, or surgical sperm retrieval to facilitate ART.
In essence, ejaculatory disorders, once carefully categorized, often yield to intervention, ensuring patients still have viable options for paternity.
Libido and Hormonal Dysfunction
The Role of Testosterone
Low libido often reflects a hormonal underpinning, most commonly testosterone deficiency. Surveys suggest up to 50% of infertile men with oligozoospermia present with hypogonadism. Yet not every patient with low testosterone will benefit meaningfully from hormone therapy, particularly if erectile dysfunction is the presenting symptom.
The therapeutic paradox is well known: while exogenous testosterone can restore libido and energy, it suppresses spermatogenesis through negative feedback on the hypothalamic-pituitary-gonadal axis. In men actively seeking fertility, this is an unacceptable trade.
Alternatives to Testosterone Replacement
Fortunately, several pharmacologic strategies allow testosterone optimization without impairing spermatogenesis:
- Selective estrogen receptor modulators (SERMs), such as clomiphene citrate, enhance endogenous gonadotropin production.
- Aromatase inhibitors reduce estradiol conversion, raising testosterone levels.
- Human chorionic gonadotropin (hCG) directly stimulates testicular Leydig cells.
Each requires close monitoring, but all preserve fertility potential while addressing symptomatic hypogonadism.
Clinical Evaluation
Assessing libido requires careful, often sensitive questioning. Validated tools such as the Androgen Deficiency in Aging Male questionnaire may help, but honest conversation is often the best diagnostic tool. Clinicians must differentiate between decreased desire caused by hormonal insufficiency and that caused by psychological stressors, relationship issues, or the relentless scheduling of intercourse demanded by infertility treatment.
Psychological Stress and Sexual Dysfunction
The Emotional Weight of Infertility
While much of reproductive medicine focuses on hormones and gametes, the psychological burden of infertility should never be underestimated. Studies consistently reveal elevated anxiety, loss of sexual enjoyment, and reduced self-esteem among men in infertile partnerships. Roughly 21% of men report high levels of infertility-related sexual stress.
This stress does not merely coexist with dysfunction—it exacerbates it. Erectile difficulties become more frequent, premature ejaculation more severe, and libido more fragile when every act of intimacy carries the pressure of conception.
Integrating Psychological Care
For the reproductive urologist or infertility specialist, referral to mental health professionals should not be an afterthought but a routine part of care. Psychotherapy, cognitive-behavioral interventions, and couple-focused therapy can restore intimacy beyond the confines of fertility goals.
Interestingly, some studies show that long-term sexual satisfaction remains stable in couples regardless of whether they ultimately conceive, provided they receive adequate psychological support.
A Holistic Perspective
Addressing male infertility therefore requires a biopsychosocial model. Without acknowledging the psychosocial dimension, treatment remains incomplete, and the vicious cycle of dysfunction continues.
Clinical Conclusions
The evaluation of sexual dysfunction in infertile men is not a tangential pursuit; it is central to both reproductive success and overall male health. Erectile dysfunction, ejaculatory disorders, and low libido are not only obstacles to conception but also potential indicators of serious comorbidities, from diabetes to cardiovascular disease.
The physician’s responsibility is to investigate diligently, treat comprehensively, and counsel compassionately. For some men, the path involves PDE5 inhibitors or SSRIs; for others, lifestyle modification or sperm retrieval. For all, it involves reassurance that their condition is treatable, their masculinity intact, and their hope for fatherhood still viable.
FAQ: Male Sexual Dysfunction and Infertility
1. Can erectile dysfunction alone cause infertility?
Yes. Since an erection is necessary for vaginal penetration and semen deposition, persistent ED can prevent conception. However, ED also often signals underlying vascular or metabolic disease, so evaluation may uncover other health concerns.
2. Why is testosterone therapy not recommended for men trying to conceive?
Exogenous testosterone suppresses the hypothalamic-pituitary-gonadal axis, lowering intratesticular testosterone and impairing spermatogenesis—sometimes to the point of azoospermia. Fertility-preserving alternatives such as SERMs, aromatase inhibitors, or hCG are preferable.
3. What options exist for men with retrograde ejaculation?
First, causative medications should be discontinued if possible. Alpha agonists or tricyclic antidepressants may restore bladder neck closure. If unsuccessful, sperm retrieved from post-ejaculatory urine can be used for assisted reproduction.


