Introduction: The Unyielding Challenge of Megaesophagus
Among the many conditions that challenge veterinary medicine, canine megaesophagus (ME) stands out for its combination of pathophysiologic complexity and clinical frustration. ME, characterized by dilated, hypomotile, and poorly functional esophageal musculature, is the most common cause of regurgitation in dogs. The disorder leads to chronic nutritional compromise, weight loss, aspiration pneumonia, and—perhaps most demoralizingly for owners—an often grim prognosis despite tireless care.
For decades, the management of ME has been largely palliative. Veterinarians have relied on elevated feeding, gravity-assisted posturing (the iconic “Bailey chair”), and customized diet consistencies to help ingesta reach the stomach. Pharmacologic innovation, on the other hand, has lagged behind. No single medication has yet demonstrated reliable efficacy in restoring esophageal motility or preventing regurgitation.
This therapeutic void inspired a group of researchers at Washington State University’s College of Veterinary Medicine to test an intriguing candidate: sildenafil, the phosphodiesterase-5 inhibitor better known for its vascular and smooth muscle–relaxing effects. Could a drug designed to treat pulmonary hypertension and erectile dysfunction possibly aid esophageal clearance in dogs?
In their randomized crossover study, the team explored whether compounded liquid sildenafil, delivered orally, could improve clinical and physiologic outcomes in dogs with generalized ME. The results, while nuanced, open a fascinating conversation about the intersection of pharmacology, motility disorders, and realistic expectations in veterinary care.
Understanding Megaesophagus: A Physiologic Dead End
The Mechanics of Failure
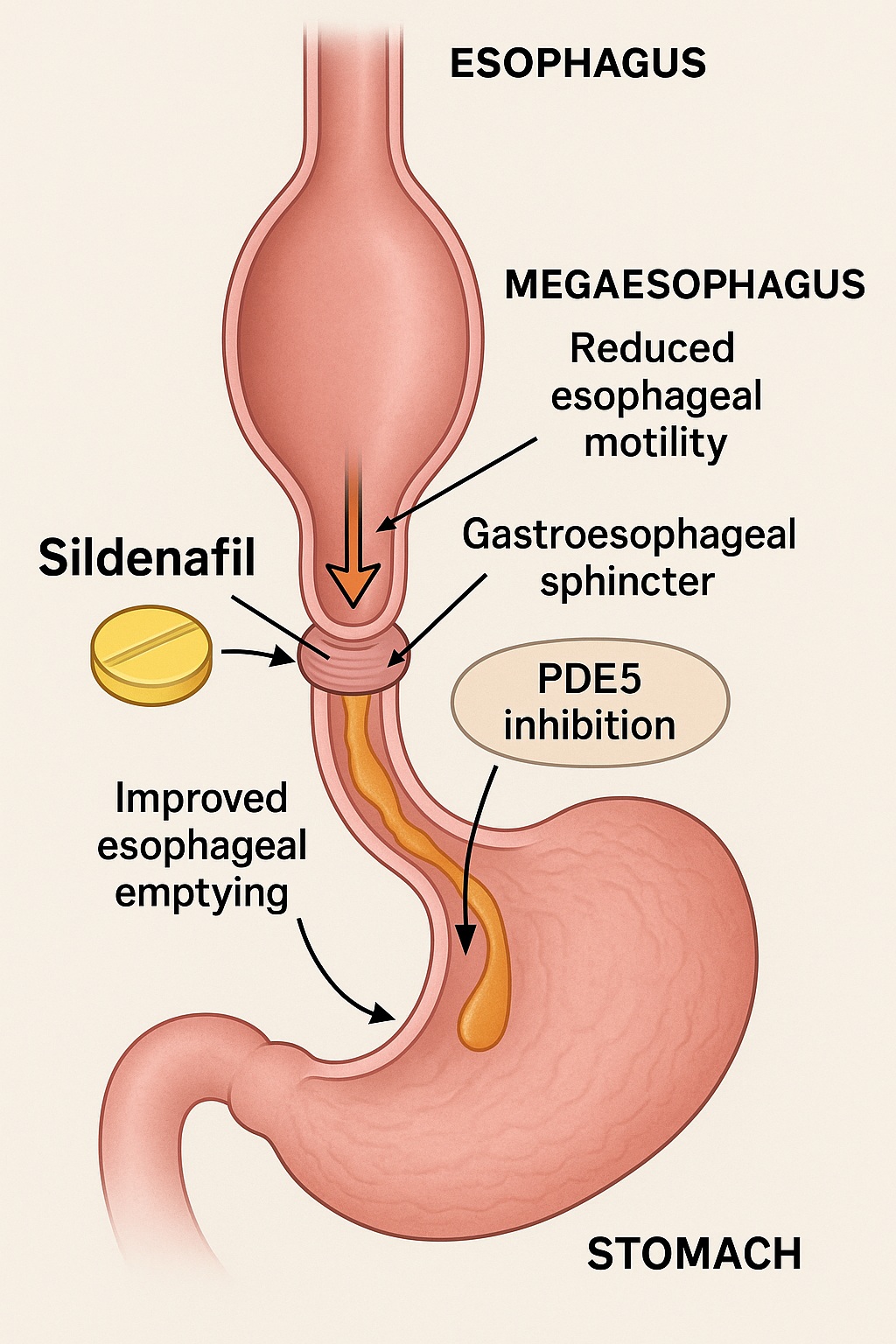
The normal canine esophagus functions as a finely tuned conduit: coordinated peristaltic waves propel food boluses from the pharynx to the stomach, aided by precise relaxation of the gastroesophageal sphincter (GES). In ME, this coordination collapses. The esophagus becomes flaccid and dilated, often losing peristaltic capability altogether. Material accumulates, leading to regurgitation—a passive ejection of undigested contents without warning or effort.
The causes of ME are diverse. Congenital cases are frequently idiopathic, reflecting developmental neuromuscular immaturity, while acquired forms can result from myasthenia gravis, hypothyroidism, esophagitis, or systemic neuromuscular disease. Regardless of etiology, the result is the same: inefficient propulsion and stasis of ingesta, predisposing to malnutrition and aspiration pneumonia.
The Prognostic Problem
Statistics are sobering. Previous studies report median survival times of one to three months after diagnosis, with overall mortality exceeding 70%. The fatal cascade typically involves recurrent aspiration, progressive weight loss, and owner fatigue with lifelong feeding regimens. Even in well-managed cases, maintaining body condition and preventing complications require meticulous care.
Given this bleak outlook, any intervention capable of improving esophageal transit—even marginally—deserves attention. This is where sildenafil, with its potential to relax the GES and facilitate gastric entry, comes under scrutiny.
The Sildenafil Hypothesis: From Achalasia to Megaesophagus
Lessons from Human Medicine
In human gastroenterology, sildenafil has been studied for achalasia, a primary esophageal motor disorder defined by impaired peristalsis and failure of GES relaxation. Through selective inhibition of phosphodiesterase-5 (PDE-5), sildenafil enhances cyclic guanosine monophosphate (cGMP) signaling, leading to smooth muscle relaxation.
Clinical studies have demonstrated that sildenafil reduces GES tone within minutes of administration, with effects lasting approximately one hour. This short-acting relaxation can facilitate esophageal emptying in achalasia patients. Translating this mechanism to dogs with ME is conceptually attractive, even though canine ME typically lacks overt GES hypertonicity. The hope is that by transiently softening the sphincter barrier, more food could reach the stomach before regurgitation occurs.
Why Liquid Formulation?
Tablets and capsules risk lodging within a flaccid esophagus, posing both inefficacy and danger. A liquid formulation ensures smoother passage and more uniform dosing. The compounded beef-flavored sildenafil used in this study, at 1 mg/kg every 12 hours, was designed to mimic real-world veterinary practice—though, as we will see, compounding introduces its own challenges.
Study Design: The Crossover Approach
Participants and Protocol
Ten client-owned dogs with stable, previously diagnosed ME were enrolled, representing a mix of breeds and etiologies. Each dog acted as its own control in a randomized crossover design: two 14-day treatment periods (sildenafil vs. placebo) separated by a 7-day washout.
Owners meticulously logged regurgitation frequency and subjective quality-of-life scores, while veterinarians performed videofluoroscopic evaluations to measure esophageal clearance times for liquid and slurry meals. Body weight served as an objective proxy for nutritional improvement.
The Imaging Setup
Dogs were positioned upright in Bailey chairs, an arrangement that allowed gravity to assist esophageal transit during imaging. Contrast material (iohexol diluted with broth) visualized the movement of fluids and food through the esophagus and into the stomach. This setup offered a non-invasive, repeatable window into esophageal function—without the discomfort or sedation required for manometric studies.
The Statistical Lens
The study was powered to detect a five-minute difference in esophageal clearance time between treatments. Non-parametric analyses (Wilcoxon tests) were applied to regurgitation frequency, body weight, and quality-of-life scores, ensuring robustness against the small sample size and non-normal data distribution.
Results: Small Steps, Subtle Shifts
Regurgitation Frequency
Sildenafil administration produced a statistically significant reduction in regurgitation episodes—from a median of 6.5 per week at baseline to 3.5 per week during treatment. The placebo period showed a slight improvement (median 4 episodes per week) but did not reach statistical significance.
However, the authors noted that the magnitude of change—though measurable—was modest. In practical terms, many dogs experienced variability, with some improving markedly while others showed no difference or even mild worsening.
Body Weight Changes
Body weight increased modestly after sildenafil therapy (median +2.35%), reaching statistical significance compared with baseline. No significant weight change occurred with placebo. This finding supports the intuitive link between reduced regurgitation and improved caloric retention, a critical outcome for dogs battling chronic malnutrition.
Esophageal Clearance
Videofluoroscopy revealed no significant differences in clearance times between sildenafil, placebo, and baseline conditions. The median clearance hovered around 25 minutes in all groups—a reminder that even pharmacologic relaxation of the GES cannot compensate for profound esophageal hypomotility upstream. Interestingly, sildenafil reached the stomach in only 70% of sessions, underscoring the unpredictability of liquid transit in ME patients.
Quality of Life
Owners rated their dogs’ quality of life as good or excellent at baseline, leaving limited room for perceived improvement. Unsurprisingly, no significant changes were detected after either treatment. Five owners correctly guessed when their dog was on sildenafil; three guessed incorrectly, and two could not tell—a testament to the subtlety of any clinical effect.
Discussion: Between Promise and Practicality
The Glimmers of Benefit
The study’s findings hint at a cautious optimism. Fewer regurgitation events and modest weight gain are clinically meaningful for some dogs, especially when viewed against the condition’s grim natural history. For patients teetering between malnutrition and stability, even incremental improvements may justify continued therapy.
Moreover, tolerability was excellent. No dogs experienced adverse effects, a notable achievement given sildenafil’s systemic actions. The dosage—1 mg/kg twice daily—appears safe and practical for long-term administration under veterinary supervision.
The Mechanistic Limitations
Despite these small victories, the pathophysiologic reality remains: ME is primarily a disorder of motility, not sphincter tone. Sildenafil’s influence on the GES cannot restore absent peristalsis. Its potential benefit likely derives from improved gastric entry of liquids that have already reached the distal esophagus, not from enhanced propulsion of material through a flaccid tube.
The fact that sildenafil failed to significantly alter clearance times supports this interpretation. In many dogs, the medication itself never reached the stomach before feeding, preventing absorption and pharmacologic action. This reinforces a key lesson: drug delivery in ME is as much a challenge as drug selection.
Compounding Complexities
An unexpected twist emerged when the researchers discovered that their liquid sildenafil was compounded from bulk sildenafil powder, not an FDA-approved drug product. While common in veterinary compounding, this practice introduces uncertainty in purity, potency, and bioavailability. Variability in drug concentration could easily blur any real effects, positive or negative.
Clinicians should therefore exercise caution, ensuring that compounded medications originate from approved finished products. Otherwise, well-intentioned therapies may become unintentional experiments.
Clinical Interpretation: When Less Is Still Something
Individual Variability
Perhaps the most telling insight is that response to sildenafil varied dramatically between dogs. Some experienced substantial improvement in regurgitation frequency; others did not. This heterogeneity likely reflects differences in esophageal geometry, GES compliance, residual motility, and even feeding practices.
It is plausible that a subset of dogs—those with partial distal motility or transient GES dysfunction—derive genuine benefit, whereas those with severe generalized atony do not. Identifying these subpopulations should be a priority for future trials.
The Role of Owner Management
In chronic conditions like ME, owner diligence often outweighs pharmacology. Consistent feeding posture, meal texture, and timing are powerful determinants of outcome. Even the best-designed medication cannot overcome sloppy adherence to gravity-assisted protocols. The study’s participants, by virtue of enrollment, likely represented highly motivated owners—possibly masking the drug’s relative impact.
The Cost-Benefit Equation
Sildenafil is neither cheap nor curative. Its routine use should therefore be individualized. In dogs where regurgitation remains severe despite optimal management, a therapeutic trial may be justified, provided the owner understands that results are unpredictable and improvements may be subtle. For mild cases with stable weight and good quality of life, observation and supportive care may suffice.
Scientific Reflections: Lessons Beyond the Data
The Power and Limits of Small Studies
Ten dogs, two treatment phases, countless data points—and yet, no definitive verdict. Such is the nature of early-phase translational research. The crossover design is elegant, minimizing inter-subject variability, but small sample size inevitably limits statistical power. Still, even modest studies like this one lay crucial groundwork for hypothesis refinement and dose optimization in future research.
The Value of Negative Findings
In academia, “negative” results often carry hidden insight. The absence of a dramatic improvement underscores the multifactorial nature of ME. It reminds clinicians that expecting a single pharmacologic “fix” for a structural-functional disorder may be unrealistic. The study contributes meaningfully by delineating where sildenafil does not work as much as where it might.
Toward Precision Veterinary Medicine
Imagine a future where each ME patient undergoes functional imaging and motility mapping before therapy—identifying those with preserved distal activity who could respond to GES relaxants. Pair this with standardized compounding, pharmacokinetic monitoring, and AI-driven prediction models, and what now seems modest could become transformative. The current study is merely the first stepping stone toward such precision.
Practical Guidance for Clinicians
Veterinarians considering sildenafil for canine ME should observe several principles:
- Confirm diagnosis and stability before initiating therapy; rule out treatable secondary causes such as myasthenia gravis or hypothyroidism.
- Use only legally compounded or approved formulations, ideally derived from FDA-certified sildenafil citrate tablets or suspensions.
- Administer in upright posture, followed by feeding within 2–5 minutes to enhance gastric transit.
- Monitor for clinical response—not just by counting regurgitation events but by tracking body weight, appetite, and owner satisfaction.
- Reassess necessity after a 2- to 4-week trial; discontinue if no meaningful benefit is observed.
Ultimately, sildenafil should be seen as an adjunctive experiment in hope, not a replacement for the mechanical diligence that underpins ME management.
Limitations and Ethical Context
The authors candidly acknowledged limitations: small sample size, unmeasured GES pressures (due to the impracticality of manometry in awake dogs), reliance on owner-reported data, and the confounding effects of compounding variability. These factors, while unavoidable, highlight the ethical balancing act in veterinary trials—pursuing scientific rigor without compromising animal welfare or owner cooperation.
Furthermore, the study’s reliance on upright positioning may have prevented the observation of potential adverse effects such as gastroesophageal reflux, which could theoretically worsen with excessive sphincter relaxation. Longer studies, incorporating esophageal pH monitoring and serum pharmacokinetics, could address these gaps.
Conclusion: Hope, Caution, and the Long Road Ahead
The Washington State University team has provided the veterinary community with something rare: controlled, evidence-based insight into a disease long governed by anecdote and improvisation. Their findings suggest that liquid sildenafil may modestly reduce regurgitation frequency and support weight gain in some dogs with ME—without adverse effects. Yet the improvements were small, inconsistent, and statistically fragile.
In other words, sildenafil is not a miracle, but perhaps a helpful whisper in a disease defined by silence of motility. Its clinical role will likely remain selective, reserved for motivated owners and patients who can tolerate the regimen.
Still, the study’s broader contribution transcends the drug itself. It illustrates the value of rigorous, humane veterinary research, encourages critical scrutiny of compounding practices, and rekindles hope that even chronic, fatal conditions can yield to science—if only incrementally.
FAQ: Key Questions About Sildenafil Use in Canine Megaesophagus
1. Does sildenafil cure canine megaesophagus?
No. Sildenafil does not restore esophageal motility or cure the underlying disorder. It may, in some dogs, reduce regurgitation frequency by relaxing the gastroesophageal sphincter and facilitating gastric emptying.
2. Is liquid sildenafil safe for dogs?
Yes, at doses around 1 mg/kg twice daily, sildenafil is generally well tolerated, with no significant adverse effects reported in controlled studies. However, compounding quality and source material are critical—only use products derived from FDA-approved formulations.
3. Should all dogs with ME receive sildenafil?
Not necessarily. The drug may benefit certain individuals but offers limited or no improvement in others. Veterinarians should consider a short therapeutic trial under close monitoring and continue only if measurable benefit occurs.