Introduction
Erectile dysfunction (ED) has long since outgrown its reputation as a whispering taboo of the bedroom. Once shrouded in embarrassment, it is now recognized as a major public health issue affecting physical, psychological, and relational well-being. Estimates suggest that ED affects over 150 million men worldwide, with prevalence projected to double by 2025. Beyond sexual dissatisfaction, ED frequently serves as a sentinel symptom of systemic diseases such as cardiovascular disease, diabetes mellitus, hypertension, and endocrine disorders.
Pharmacological interventions, particularly phosphodiesterase type 5 (PDE5) inhibitors, have transformed the therapeutic landscape of ED. However, the accessibility and appropriate use of such agents are critically dependent on the pharmacy workforce, particularly in countries where community pharmacies often act as the first point of contact for patients. Pharmacists and pharmacy technicians, therefore, represent not only dispensers of medicines but also gatekeepers of safe and rational ED management.
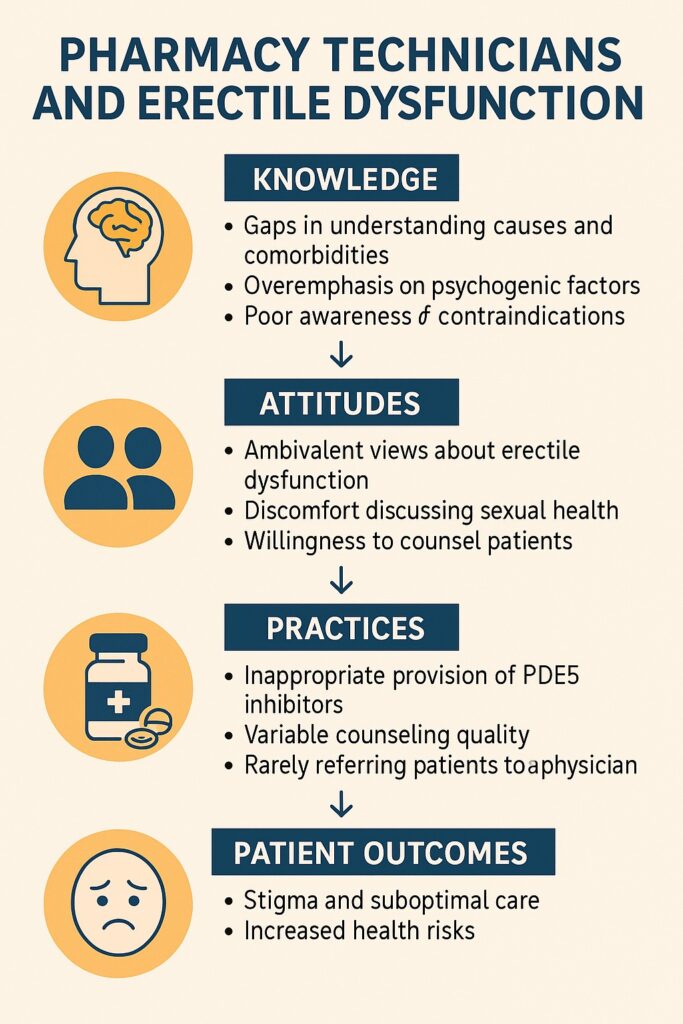
A recent 2024 study conducted in Gondar Town, Northwest Ethiopia, sought to illuminate precisely this issue: what do pharmacy technicians know about ED, what attitudes do they hold, and how do they practice when faced with ED-related consultations? The findings are revealing, occasionally concerning, and certainly instructive for shaping health policy, education, and professional practice.
The Centrality of Community Pharmacies in Men’s Health
Community pharmacies occupy a unique position in healthcare delivery, particularly in low- and middle-income countries. They are accessible, affordable, and less intimidating than hospital settings, making them the first stop for many men hesitant to disclose intimate health concerns. In Ethiopia, pharmacy technicians frequently operate independently, providing advice, dispensing medications, and shaping patient perceptions of disease and treatment.
When it comes to ED, the role of these professionals becomes even more critical. Patients may bypass physicians altogether, opting for over-the-counter remedies, herbal products, or informally dispensed PDE5 inhibitors. This places enormous responsibility on pharmacy technicians to:
- Correct misconceptions surrounding ED.
- Recognize red flags that warrant referral to physicians (e.g., sudden onset ED, comorbid cardiovascular disease).
- Ensure safe dispensing practices, avoiding contraindicated combinations such as PDE5 inhibitors with nitrates.
The study from Gondar highlights how well (or poorly) these responsibilities are being met in real-world practice.
Knowledge: What Do Pharmacy Technicians Know About ED?
The Gondar study revealed gaps in baseline knowledge among community pharmacy technicians. While most participants were aware that ED is common and multifactorial, many struggled to identify its underlying causes accurately. Cardiovascular disease and diabetes—two of the most robustly documented etiologies—were inconsistently recognized. Instead, a subset of respondents overemphasized psychological stress as the predominant cause, underestimating the biological underpinnings.
When asked about pharmacotherapy, awareness of PDE5 inhibitors such as sildenafil was nearly universal. However, fewer technicians demonstrated knowledge of contraindications, dose adjustments, or side effect profiles. Alarmingly, some respondents considered PDE5 inhibitors safe for use without medical consultation, overlooking the potentially fatal interaction with nitrates or the risks in patients with uncontrolled hypertension.
Knowledge of alternative or adjunctive therapies, such as lifestyle modification (weight loss, exercise, smoking cessation), was limited. This knowledge gap diminishes the potential of pharmacy technicians to promote holistic care, reducing them to mere pill dispensers rather than true healthcare partners.
Attitudes: How Do Pharmacy Technicians Perceive ED and Its Management?
Attitudes matter. A technician who perceives ED as a trivial inconvenience will counsel patients very differently than one who views it as a window into systemic disease. In Gondar, attitudes were a mixed bag.
On the positive side, most participants acknowledged that ED negatively impacts quality of life and marital harmony. They expressed willingness to provide counseling and demonstrated empathy toward patients seeking advice. Such openness is commendable in a cultural context where sexual health remains a sensitive topic.
Yet, a subset of technicians displayed dismissive or judgmental attitudes, perceiving ED consultations as embarrassing or even inappropriate. These attitudes create barriers to patient disclosure, reinforcing stigma and deterring men from seeking timely help. Additionally, the belief that ED treatment is primarily about restoring masculinity, rather than addressing holistic health, reflects a narrow lens that risks perpetuating misconceptions.
Ultimately, the study underscored the need for attitude recalibration—a reminder that pharmacy practice must integrate empathy with evidence, and professionalism with cultural sensitivity.
Practices: How Do Technicians Behave in Real-World Encounters?
Practice often reveals the truth that theory conceals. Despite gaps in knowledge and ambivalence in attitudes, pharmacy technicians in Gondar frequently engaged in active dispensing of PDE5 inhibitors. Alarmingly, many admitted to providing these medications without prescriptions, relying instead on patient request or self-reported symptoms.
While this may enhance accessibility, it introduces several risks: inappropriate self-medication, masking of underlying disease, drug–drug interactions, and even psychological dependence on PDE5 inhibitors. Few technicians consistently referred patients for medical evaluation, even when cardiovascular risk factors were evident.
Counseling practices were equally variable. Some provided instructions on timing of medication intake (e.g., sildenafil 30–60 minutes before intercourse), while others omitted key counseling points regarding avoidance of alcohol or high-fat meals that delay absorption. Lifestyle counseling was rare, and follow-up recommendations were inconsistently offered.
In short, practices often fell short of professional standards, reflecting both systemic gaps in regulation and individual deficits in training.
Predictors of Better Knowledge, Attitudes, and Practices
The study identified several predictors that influenced technician performance. Higher educational attainment, longer professional experience, and prior training in sexual and reproductive health were consistently associated with better knowledge and safer practices. Younger technicians, while more open-minded in attitudes, were often less confident in counseling due to lack of experience.
This points toward a simple yet powerful solution: structured continuing education and targeted training programs. By enhancing competence, such interventions can transform pharmacy technicians into effective allies in men’s health rather than weak links in the healthcare chain.
Implications for Policy and Practice
The Gondar findings echo a broader theme in global health: the quality of care is only as strong as the weakest link in the delivery chain. Pharmacy technicians are indispensable in regions where physicians are scarce, yet their role in ED management remains underdeveloped.
Several implications emerge:
- Educational reform: Sexual and reproductive health modules must be integrated into pharmacy technician curricula, emphasizing ED as both a quality-of-life issue and a potential marker of systemic disease.
- Continuing professional development: Regular workshops, certification courses, and case-based training can bridge existing knowledge gaps.
- Regulatory oversight: Policies should enforce prescription-only dispensing of PDE5 inhibitors, with penalties for noncompliance, while simultaneously improving referral networks.
- Public health campaigns: By collaborating with pharmacy staff, public health authorities can destigmatize ED, promote lifestyle modifications, and encourage appropriate medical consultations.
The Ethiopian context may be specific, but the lessons are universal. Pharmacy professionals everywhere must be equipped, both intellectually and attitudinally, to address ED safely and effectively.
Reflections: The Human Side of Erectile Dysfunction
At its core, ED is not merely about erections. It is about intimacy, self-esteem, and relational harmony. For patients, the first point of disclosure is often the community pharmacy—an environment less intimidating than the clinic. Whether that first disclosure leads to relief or regret depends largely on the response of the pharmacy professional.
If the technician offers empathy, accurate advice, and safe guidance, the patient steps onto a path of recovery. If, instead, the response is dismissive, judgmental, or careless, the patient may withdraw into silence, compounding both emotional distress and medical risk. In this sense, pharmacy technicians stand as quiet but critical arbiters of men’s health outcomes.
The Gondar study should therefore be read not merely as an audit of knowledge, attitudes, and practices, but as a call to elevate the standards of care for ED across all healthcare touchpoints.
Conclusion
The evaluation of pharmacy technicians in Gondar Town paints a picture that is both sobering and hopeful. Knowledge gaps, attitudinal biases, and unsafe dispensing practices currently undermine the potential of community pharmacies as safe havens for men with erectile dysfunction. Yet, the predictors of improvement—education, training, and professional development—are tangible, achievable, and well within reach.
Erectile dysfunction deserves more than superficial attention. It is both a symptom and a disease, both a medical and a psychosocial challenge. Empowering pharmacy technicians with accurate knowledge, empathetic attitudes, and safe practices can transform community pharmacies into pivotal allies in the fight against ED.
FAQ
1. Why is it risky for pharmacy technicians to dispense sildenafil without a prescription?
Because ED may be a symptom of underlying cardiovascular or endocrine disease, dispensing sildenafil without medical evaluation risks masking serious conditions. Moreover, PDE5 inhibitors can interact dangerously with nitrates and other medications.
2. What should pharmacy technicians do when a patient requests ED medication?
They should provide empathetic counseling, assess red flags, educate about lifestyle modifications, and refer the patient to a physician for proper diagnosis. Dispensing without prescription should be avoided.
3. Can training really improve pharmacy technicians’ handling of ED?
Yes. The study demonstrated that technicians with more education and prior training in sexual health displayed better knowledge, attitudes, and practices. Structured training programs are therefore an effective solution.


