Getting Your Prescriptions Approved
Most people with Blue Cross NC health insurance also have a drug plan to cover the drugs they get at their pharmacy. Each drug plan comes with a list (also known as a formulary) that shows you what drugs are covered.
Are your prescription drugs covered?
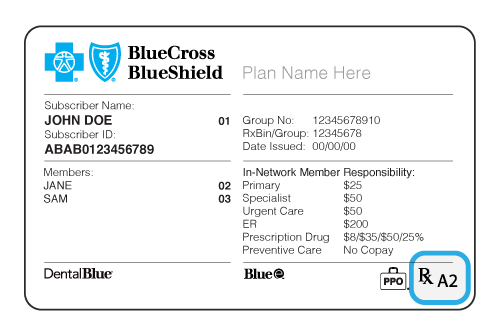
1) Look for the “Rx” on the front of your Blue Cross NC member ID card. It means you have drug coverage.
2) Look for a capital letter or a capital letter/number combination after the “Rx” on your card. The letter will tell you which drug list, or formulary, your plan uses. The number gives information about the pharmacies in your network.
Enhanced Drug List
A, B,
Essential Drug List
C, D
Net Results Drug List
E
How to Find Your Approved Drugs List or Formulary
1) Log in to Blue Connect or register for an account at https://www.bcbsnc.com/members/public/register/
Already logged in? Skip to step 2.
2) Go to the Prescriptions page
Click Find a Drug, then Search for Prescription Drugs – Prime Therapeutics
Prime Therapeutics is our pharmacy benefits website. Your drug list (or formulary) name should look like this:

3) Search for your prescription drug
Type a drug name in the blue search box and Submit. The drug name, description and cost info will appear under “Selected medicines.” If you need prior authorization or have other special requirements, that may be listed here also.
Drugs that Need Prior Authorization
What is Prior Authorization? This means your doctor must explain in writing why you need a certain medication before Blue Cross NC can decide if it will be covered.
Our drug search tool shows the restricted drugs our members use most, and the details your doctor or provider must send us to get them approved.
Enter your drug name in the search box to see if it needs approval before it’s covered under your plan.
- A
- B
- C
- D
- E
- F
- G
- H
- I
- J
- K
- L
- M
- N
- O
- P
- Q
- R
- S
- T
- U
- V
- W
- X
- Y
- Z
Brand Drug Name: <
>
- Generic Drug Name:
- Benefit: ,
- Specialty:
- Prior Review Required On : ,
Words that you may see in the drug search
Prior Authorization
Your doctor must explain in writing why you need a certain medication before Blue Cross NC can decide if it will be covered.
Supply or Quantity Limits
To encourage the proper use of prescription drugs, Blue Cross NC may restrict the amount of medicine your insurance plan covers. This may mean taking fewer pills each day without changing the total amount of medication.
Step Therapy
Blue Cross NC requires that you first try a drug or device that is not restricted before a restricted drug will be approved. You may be covered for a restricted drug if your doctor tells Blue Cross NC in writing that:
- You have already used the non-restricted drug, and it wasn’t effective in treating the condition; or
- If your doctor thinks the non-restricted drug is likely to be harmful to your health or not effective in treating your condition.
Non-formulary*
A non-formulary drug is one that isn’t on your Blue Cross NC drug list. Not all drug lists or formularies have non-formulary drugs. Doctors must confirm that you have tried a drug on your list first and that they were ineffective or harmful to you. Also, medication-specific clinical criteria must be met before approval (available in the Drug Search).
Specialty Drugs*
May be used to treat a complex or rare condition, and are generally:
- Prescribed with special dosing or administration
- Prescribed by a specialist
- Significantly more expensive than alternative therapies
Specialty drugs are limited to a 30-day supply and you must get them from an in-network specialty pharmacy, so your benefits will apply to the prescription. In-network pharmacy options vary based on your plan benefits.
*See “Covered Services” and “Glossary” in your benefit booklet for to learn more.
Members with Essential Drug Lists or Formularies: If you meet certain conditions, read the Criteria for Approval of Restricted Products (pdf), and your list says that Prior Review (Prior Authorization) or Step Therapy is required for a drug, but the drug isn’t in the Drug Search, have your doctor send your information to Blue Cross NC using this General Authorization Fax Form (pdf).
Important: If you’ve changed health plans, your doctor or provider may need to tell us that you’ve met the rules for your new plan.
Requesting Drugs Not on Your Approved Drugs List (Formulary)
For Fastest Processing, have a doctor or provider submit your request directly to Blue Cross NC.
If you submit the request yourself, it will take longer to process while we contact your provider to get the information needed. They have 5 calendar days to respond.
- Online (Preferred – for Providers Only):CoverMyMeds.com Some drugs if approved can be ready at the pharmacy in less than 2 hours.
- Mail: Blue Cross NC, Attn: Corporate Pharmacy, P.O. Box 2291, Durham, NC 27707
- Phone: 800-672-7897
- Fax: 800-795-9403
- Email:[email protected]Important! Sending health information by email comes with the risk that it could be read by people you didn’t send it to. Use an encrypted email service or other secure means of communication that may protect your information from third parties. You acknowledge that you understand these risks when you send your email.
All requests must include:
- Patient’s name, date of birth, gender and phone number
- Member’s Blue Cross NC ID number
- Name of the drug
- Doctor’s name and phone number
Once we have all your information, we’ll make a decision within 3 business days and notify your doctor. Requests are processed within 72 hours, unless urgent.
Urgent requests are handled within 24 hours. An urgent request is when the prescriber thinks a delay would seriously jeopardize the life or health of the patient, the patient’s ability to regain maximum function, or would subject the patient to severe pain that cannot be adequately managed without the care or treatment requested.
Authorization for Essential Formulary Medications
If your doctor or provider wants you to take a drug that isn’t on your Essential drug list, here’s what to do:
- Ask if there’s another drug you could take.
- Check to see if the new drug is on your drug list. If you can use another drug, you’re all set!
- If you still need the non-formulary drug, have your provider send us a request to approve the non- formulary drug.
- For approval, you must meet your plan’s Non-Formulary Exception Criteria (pdf). If the drug is listed in the Drug Search, these requirements may still apply.
- Your doctor or provider must send all your details, and their signature, on the General Authorization QL Fax Form (pdf) to Blue Cross NC.
- For questions, or to check the status of your review, call us at 1-800-672-7897.
Cost Information for Essential and Net Results
For members on the Essential Drug List (formulary), if your request for a non-formulary drug is approved, these cost levels or “tiers” will apply:
Essential 5 Tier = Tier 5
Essential 6 Tier = Tier 6
Drugs with Limited or No Plan Coverage
Some drugs may not be covered by your plan or may have a limited amount you can get with your plan. The Table of Drugs with Limited or No Coverage shows a sample listing. Not all limited medications are listed.
Self-funded and ASO group members should check their member guide or call Blue Cross NC Customer Service for drug limits that may apply to them.
Table of Drugs with Limited or No Coverage
For groups that had a $5,000 lifetime maximum in 2013 and were able to carry this over due to updates to the Affordable Care Act, coverage will remain available. Otherwise, limits are as follows (call Customer Service to confirm):
Underwritten and Individual/Family plans:
Infertility drugs are limited to the following lifetime maximum per member:
- Follitropins (e.g., Bravelle, Follistim, Follistim AQ, Gonal-F*) (3,000 units)
- Oral ovulation stimulants (Clomid) (360 tablets)
- Subcutaneous injectable ovulation stimulants (e.g., Ovidrel*) (1,000 micrograms)
- Subcutaneous injectable ovulation stimulants (e.g., Luveris) (1,500 units)
- Intramuscular injectable ovulation stimulants (e.g., Novarel, Pregnyl) (40,000 units)
- Menotropins (e.g., Repronex, Menopur) (1,500 units)
- Gonadotropin-releasing hormone antagonists (e.g., Cetrotide*, Ganirelix) (3mg)
- Progestins (e.g., Crinone 8%* gel) (101.25g or 90 syringes/applicators)
- Progestins (e.g., Prometrium* suppositories, Endometrin suppositories) (90 units)
*identifies drugs which require prior authorization before being covered
- Tadalafil (Cialis) 2.5mg or 5mg: 30 tablets per 30 days
- 4 tablets or units per 30 days all others
- Azeschew
- Azesco
- DermacinRx Pretrate
- Pregenna
- Prenara
- Prenatryl
- Prenatrix
- Trinaz
- Zalvit
All: Not covered; please see list for specific drugs that are not covered
Brand-Name Drugs vs. Generics
Don’t over pay! You could be charged more if you get a brand-name drug instead of a generic. If there’s a medical reason you need to take the brand-name drug, ask your doctor to: