Pulmonary arterial hypertension (PAH) remains one of the most formidable challenges in cardiovascular and pulmonary medicine. Defined by progressive elevation of pulmonary arterial pressure and relentless remodeling of the pulmonary vasculature, PAH inexorably leads to right ventricular failure and premature death. Despite significant advances—endothelin receptor antagonists, phosphodiesterase-5 inhibitors, prostacyclin analogs—the disease remains incurable, largely because current therapies target hemodynamics rather than the underlying molecular drivers of vascular pathology. Against this backdrop, the study of novel therapeutic agents capable of modulating dysfunctional molecular pathways has become essential.
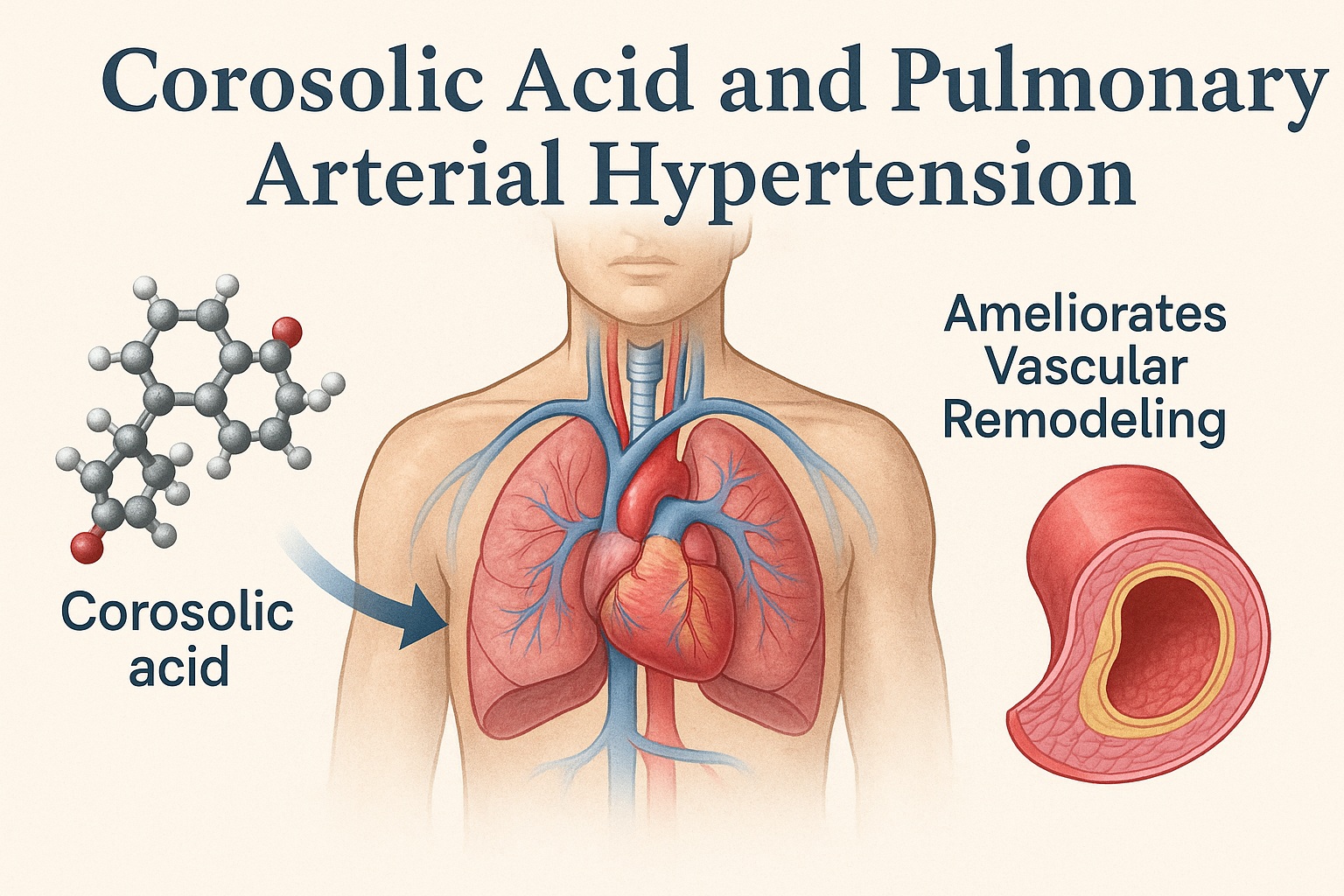
The research behind “Corosolic acid ameliorates vascular remodeling in pulmonary arterial hypertension via the downregulation of STAT3 signaling” offers a compelling contribution to this evolving field. Corosolic acid (CA)—a natural pentacyclic triterpenoid found in Lagerstroemia speciosa (banaba leaves)—has long been recognized for its anti-diabetic, anti-inflammatory, and anti-oxidant properties. Yet its potential cardiovascular and pulmonary benefits have only recently gained traction. According to the findings laid out in this study, CA may exert fundamentally protective effects in PAH by suppressing STAT3 activation, reversing pathological vascular remodeling, and attenuating right ventricular hypertrophy.
The objective of this article is to integrate those discoveries into an accessible, comprehensive, and clinically meaningful narrative—translating molecular insights into a broader medical context and highlighting CA as a promising agent in a domain where innovation is desperately needed.
PAH Pathophysiology: Why the Pulmonary Arteries Remodel Themselves Into Oblivion
Understanding the therapeutic relevance of corosolic acid first requires revisiting the core pathobiology of PAH. PAH is not merely a disorder of elevated vessel tone; it is a disease driven by aberrant cellular behavior—vascular smooth muscle cells (VSMCs) that proliferate with malignant tenacity, endothelial cells that lose normal regulatory function, and fibroblasts that invade the vascular wall with fibrotic zeal.
A central figure in this molecular drama is the STAT3 pathway. Activating STAT3 transforms ordinarily quiescent vascular cells into hyperproliferative, apoptosis-resistant entities. STAT3 increases inflammatory cytokine signaling, enhances survival pathways (particularly via Bcl-2 and survivin), and promotes migration of vascular cells. The net result is a pulmonary artery that progressively thickens, narrows, stiffens, and sabotages hemodynamics.
The study reminds us that vascular remodeling in PAH is not limited to medial hypertrophy. It also includes:
- Endothelial dysfunction, driven by oxidative stress, reduced nitric oxide, and inflammatory infiltration.
- Adventitial fibrosis, marked by excessive collagen deposition and fibroblast expansion.
- Inflammatory microenvironment formation, in which cytokines like IL-6 further activate STAT3.
This combination creates a self-reinforcing loop of vascular destruction. Current PAH pharmacotherapies rarely address these cellular maladaptations directly; instead, they modulate vasodilation. Breaking the STAT3-driven cycle would mark a true paradigm shift.
Corosolic Acid: A Natural Molecule With Remarkable Pharmacologic Versatility
Corosolic acid has attracted attention for its diverse biological properties. Historically used in traditional medicine for metabolic regulation, CA has demonstrated:
- anti-inflammatory effects through NF-κB modulation
- anti-oxidant activity reducing ROS burden
- anti-cancer properties by inhibiting proliferative signaling
- metabolic regulation through AMPK activation
These broad effects intersect strikingly with the known drivers of PAH. The present study positions CA not as a narrowly targeted agent but as a molecule that influences several aspects of pulmonary vascular pathology simultaneously—an attractive quality in a disease with complex cellular dysregulation.
The authors emphasize that CA has good bioavailability, low toxicity, and a favorable safety profile, making it an intriguing candidate for chronic therapy. Importantly, CA’s chemical structure allows it to modulate intracellular signaling cascades without the severe adverse effect burden associated with many chemotherapeutics.
While further pharmacokinetic studies are needed, CA’s natural origin and multi-pathway activity create a solid rationale for deeper exploration.
STAT3: A Master Regulator of Vascular Remodeling and a Prime Therapeutic Target
The crux of the article lies in elucidating corosolic acid’s effects on STAT3 signaling—a pathway implicated not only in PAH but in cancer, inflammation, and fibrosis. In PAH, STAT3 activation drives expression of genes that promote proliferation, migration, and resistance to apoptosis in pulmonary artery smooth muscle cells (PASMCs).
The study demonstrates that in monocrotaline-induced PAH (a widely used experimental model), STAT3 phosphorylation is dramatically upregulated in pulmonary arteries. This correlates with the structural changes evident on lung histology: thickened medial layers, narrowed lumens, and proliferative cellular infiltrates. Treatment with corosolic acid markedly reduces STAT3 activation, which corresponds to improved vascular morphology.
Corosolic acid appears to suppress STAT3 through two potential mechanisms:
- Inhibition of upstream cytokine signaling, particularly IL-6–JAK interactions.
- Direct downregulation of STAT3 phosphorylation, reducing its nuclear translocation and gene regulatory activity.
By disrupting this pathway, CA decreases the expression of proliferative proteins like cyclin D1, survival proteins like survivin, and pro-inflammatory mediators. This helps restore the balance between cellular proliferation and apoptosis.
The study elegantly illustrates this process through immunohistochemistry photos, where CA-treated lung tissues show visibly reduced STAT3 staining—highlighting the drug’s molecular precision.
To unify this mechanistic insight with clinical relevance: targeting STAT3 directly addresses the root cause of pulmonary vascular remodeling, something current PAH medications do not do.
Animal Model Findings: Corosolic Acid Reverses the Structural Signature of PAH
Using a monocrotaline model (MCT-induced PAH), the study evaluates corosolic acid’s therapeutic effect across multiple anatomical and molecular endpoints. This model reliably induces severe pulmonary hypertension through endothelial injury, inflammation, and subsequent vascular remodeling.
Hemodynamic Improvements
The article presents compelling data: CA significantly reduces right ventricular systolic pressure (RVSP), a direct indicator of pulmonary arterial load. High RVSP reflects advanced PAH; its reduction shows clear therapeutic benefit.
In CA-treated animals, RVSP values move markedly closer to those of controls, indicating a real change in vascular resistance—not merely superficial biochemical alterations.
Vascular Remodeling Reversal
CA reduces:
- medial wall thickness
- muscularization of small pulmonary arteries
- inflammatory cell infiltration
On histological images (H&E and α-SMA staining), CA-treated rats display dramatically thinner pulmonary artery walls compared to untreated PAH rats. The investigators confirm this through quantification, demonstrating highly significant reductions.
Right Ventricular Hypertrophy Attenuation
Right ventricular hypertrophy (RVH) is the clinical consequence of increased pulmonary load, and RVH reversal is a critical therapeutic target. CA treatment reduces RV/(LV+S) ratios, signaling that the right ventricle is no longer under the same pressure burden.
This finding makes CA particularly noteworthy: unlike vasodilators that improve vessel tone transiently, CA improves underlying vascular structure, thus reducing long-term cardiac stress.
Molecular Signatures of Repair
The study correlates improved hemodynamics with reduced expression of STAT3, cyclin D1, PCNA, and other proliferative markers. Simultaneously, CA enhances expression of apoptotic regulators that push dysfunctional PASMCs toward programmed cell death.
In short, CA does not simply pause disease progression—it begins to unwind pathological remodeling.
Anti-Inflammatory and Anti-Oxidant Effects: Complementary Mechanisms That Amplify Therapeutic Benefit
One of the strongest advantages of corosolic acid is its multi-dimensional activity. PAH is not driven solely by proliferation; it arises in part from chronic inflammation and oxidative stress. The study’s biochemical assays reveal that CA:
- suppresses IL-6, TNF-α, and other pro-inflammatory mediators
- reduces ROS production
- enhances endogenous anti-oxidant enzymes (e.g., SOD, catalase)
These changes reflect a healthier pulmonary environment where endothelial function can recover and smooth muscle cells are no longer bombarded by inflammatory signals.
The immunohistochemistry images in the article clearly show reduced inflammatory infiltration in CA-treated lung tissue, illustrating this systemic benefit visually.
Given inflammation’s central role in PAH progression, these secondary benefits may enhance CA’s impact beyond STAT3 inhibition.
Cellular Mechanisms: Why PASMCs Respond So Favorably to Corosolic Acid
The in vitro portion of the study investigates corosolic acid’s cellular effects on PASMCs cultured under hypoxic or IL-6–stimulated conditions. These conditions mimic the microenvironment of PAH.
Corosolic acid significantly:
- suppresses PASMC proliferation
- reduces migration behavior
- enhances caspase-dependent apoptosis
- inhibits IL-6–induced STAT3 phosphorylation
- downregulates cyclin D1, survivin, and Bcl-2
This profile indicates a profound rebalancing of PASMC behavior. Instead of resisting apoptosis and proliferating uncontrollably, CA pushes cells back toward a normal phenotype.
In a disease characterized by cellular immortality, this is a decisive therapeutic shift.
Comparison With Current PAH Therapies: Where Corosolic Acid Fits Into the Treatment Landscape
Current PAH therapies fall into three major categories:
- endothelin receptor antagonists
- phosphodiesterase-5 inhibitors
- prostacyclin analogs
These drugs improve symptoms and hemodynamics but do not reverse vascular remodeling. Their impact on long-term disease progression is therefore limited. Corosolic acid, by contrast, targets upstream molecular abnormalities—particularly STAT3—which play a causal role in remodeling.
If subsequent studies validate these findings in humans, CA could become:
- an adjunctive therapy, enhancing the effect of vasodilators
- a remodeling-targeted agent, similar in spirit to anti-fibrotic therapies
- a first-in-class STAT3 modulator for PAH
Because CA is orally bioavailable and has a strong safety profile, it may integrate more easily into chronic regimens than experimental gene therapies or monoclonal antibodies.
The article does not claim CA is ready for clinical deployment but positions it as a highly promising candidate.
Limitations and Future Directions: What Is Needed Before CA Can Enter Clinical Trials
The study acknowledges several limitations:
- reliance on a single animal model (MCT-induced PAH)
- unknown long-term toxicity in humans
- unclear optimal dosing strategies
- need for pharmacokinetic profiles in pulmonary tissue
It also highlights the need for additional mechanistic research, especially regarding:
- effects on endothelial cells
- interactions with nitric oxide signaling
- potential synergy with existing PAH treatments
Finally, human clinical trials will be required to determine whether the impressive preclinical results translate into therapeutic benefit.
Conclusion
The study presents a compelling case for corosolic acid as a novel therapeutic candidate for pulmonary arterial hypertension. By directly inhibiting STAT3 signaling—a central driver of vascular remodeling—CA addresses the molecular heart of PAH rather than merely modifying symptoms. The combination of anti-proliferative, pro-apoptotic, anti-inflammatory, and anti-oxidant effects positions CA as a uniquely multi-functional agent.
Whether corosolic acid becomes part of future PAH therapy will depend on the success of further research. Yet its potential is undeniable, and the current findings represent a meaningful contribution to the field’s ongoing search for disease-modifying treatments.
FAQ
1. Why is STAT3 such an important target in pulmonary arterial hypertension?
STAT3 drives smooth muscle proliferation, inflammation, and resistance to apoptosis—core components of vascular remodeling. Inhibiting STAT3 interrupts these pathogenic processes.
2. Is corosolic acid safe for long-term use?
CA has an excellent safety profile in existing studies, but long-term human data are lacking. Future toxicology and clinical studies are required for confirmation.
3. Could CA be combined with existing PAH medications?
Potentially yes. Because CA targets upstream molecular pathways rather than vasodilation alone, it may complement current therapies. Clinical trials would be needed to evaluate safety and synergy.