Introduction
Lower urinary tract symptoms (LUTSs) in men are among the most common and burdensome clinical complaints in urology. They affect quality of life, disrupt sleep, interfere with daily activities, and often coexist with erectile dysfunction. For decades, management was guided by a “one drug, one target” approach—alpha-blockers for voiding symptoms, 5-alpha-reductase inhibitors (5-ARIs) for prostate size reduction, and antimuscarinics for overactive bladder. However, such a linear strategy often underperforms, especially in men with mixed symptom profiles.
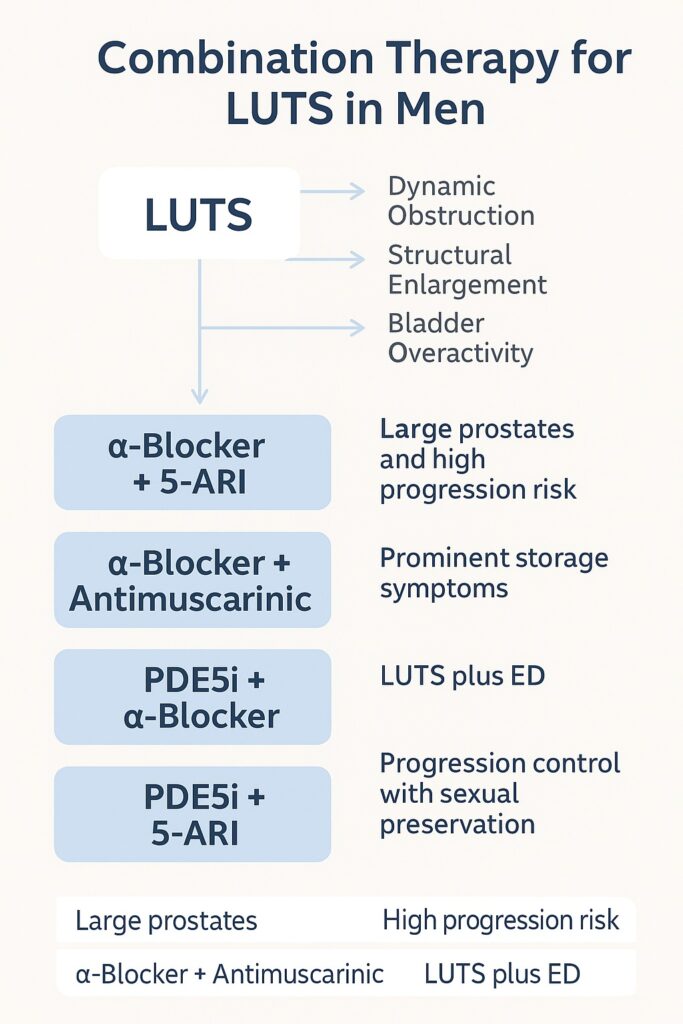
Enter combination therapy, an approach that reflects the multifactorial pathophysiology of LUTSs and the limitations of monotherapy. By addressing multiple mechanisms—dynamic obstruction, structural enlargement, bladder overactivity, and even endothelial dysfunction—combination regimens aim to maximize efficacy while balancing safety.
This article provides a comprehensive review of evidence for combination therapy in male LUTSs, exploring clinical trial data, pharmacological rationale, and practical guidance for patient selection.
Alpha-Blockers and 5-Alpha-Reductase Inhibitors
The most established combination is that of alpha-blockers (such as tamsulosin, alfuzosin, or doxazosin) with 5-ARIs (finasteride or dutasteride). This pairing reflects a logical division of labor: alpha-blockers relax smooth muscle in the prostate and bladder neck, rapidly relieving symptoms, while 5-ARIs shrink the prostate and reduce long-term risk of progression.
The MTOPS trial (Medical Therapy of Prostatic Symptoms) set the foundation by demonstrating that combination therapy significantly reduced clinical progression of benign prostatic hyperplasia (BPH) compared with either drug alone. Progression was defined broadly—worsening symptoms, urinary retention, incontinence, renal insufficiency, or recurrent infections. Notably, combination therapy reduced risk of acute urinary retention and surgery by nearly 70%.
Similarly, the CombAT study confirmed that dutasteride plus tamsulosin outperformed monotherapy in symptom relief and risk reduction. After four years, the combination achieved superior reductions in International Prostate Symptom Score (IPSS), prostate volume, and disease progression.
Yet, this efficacy comes at a cost: higher rates of adverse events such as sexual dysfunction, decreased libido, and ejaculation disorders. For some men, the prospect of symptom relief collides with a decline in sexual well-being, necessitating shared decision-making.
Alpha-Blockers and Antimuscarinics
Not all LUTSs stem from obstruction; storage symptoms such as urgency, frequency, and nocturia are often most bothersome. Here, the combination of alpha-blockers and antimuscarinics (e.g., tolterodine, solifenacin, fesoterodine) offers relief.
The rationale is straightforward: alpha-blockers improve flow, while antimuscarinics calm detrusor overactivity. Historically, urologists avoided antimuscarinics in men with LUTSs out of fear of precipitating urinary retention. However, randomized trials such as the TIMES study demonstrated that combining tamsulosin with tolterodine was not only effective but also safe, with very low rates of acute retention (<1%).
Combination therapy significantly improves storage symptoms and quality-of-life scores compared with monotherapy. Men with small to moderate prostate volumes, high frequency, and urgency are particularly good candidates.
Still, caution is advised in men with high post-void residual volumes, advanced obstruction, or history of retention. Here, careful monitoring and ultrasound assessment are indispensable.
PDE5 Inhibitors and Alpha-Blockers
The discovery that phosphodiesterase type 5 inhibitors (PDE5is), such as tadalafil and sildenafil, improve LUTSs was initially surprising. Their effect extends beyond erectile function: by enhancing nitric oxide–cGMP signaling, PDE5is relax smooth muscle in the lower urinary tract, modulate afferent nerve activity, and improve perfusion.
Clinical trials show that tadalafil improves both IPSS scores and erectile function in men with LUTSs and comorbid ED, making it a two-birds-one-stone therapy. When combined with alpha-blockers, symptom improvements are often superior to either agent alone.
The challenge lies in safety. Both PDE5is and alpha-blockers lower blood pressure through vasodilation. Though clinically significant hypotension is rare with careful dosing, the potential exists, particularly in elderly patients or those on antihypertensives. For this reason, combination therapy requires judicious titration and avoidance of high-dose short-acting PDE5is with non-selective alpha-blockers.
For men motivated by dual benefits—better urination and better erections—this regimen is particularly attractive.
PDE5 Inhibitors and 5-ARIs
An emerging but less widely adopted pairing is that of PDE5 inhibitors with 5-ARIs. Dutasteride, while effective at reducing prostate size and long-term progression, is notorious for sexual side effects. PDE5 inhibitors offer a counterbalance, preserving erectile function while improving LUTSs.
Preliminary studies indicate that tadalafil plus dutasteride improves both IPSS and sexual satisfaction compared to dutasteride alone. While long-term data remain limited, this strategy may become increasingly valuable for men seeking symptom control without sacrificing intimacy.
Clinical Decision-Making: Who Benefits Most?
The art of combination therapy lies in patient selection. Not all men require or tolerate dual regimens. The following practical principles emerge from evidence:
- Large prostates and high progression risk: Alpha-blocker + 5-ARI offers the best long-term outcomes.
- Prominent storage symptoms: Alpha-blocker + antimuscarinic improves urgency and frequency.
- LUTSs plus ED: PDE5 inhibitor alone, or PDE5i + alpha-blocker, addresses both domains.
- Progression control with sexual preservation: PDE5i + 5-ARI may strike the balance.
Equally important is recognizing when to avoid combinations—frail elderly men at risk of hypotension, patients with high residual urine, or those unable to tolerate polypharmacy.
Safety and Tolerability
Combination therapy invariably increases the risk of adverse effects. Sexual dysfunction dominates the alpha-blocker + 5-ARI landscape. Dry mouth and constipation may complicate antimuscarinic use. Hypotension can emerge with PDE5i + alpha-blockers, though rarely if properly managed.
Ultimately, the physician’s role is not to avoid combinations altogether but to anticipate risks, educate patients, and monitor closely. Shared decision-making, informed by both evidence and patient values, is the cornerstone of safe practice.
The Future of Combination Therapy
Several trends shape the horizon:
- Fixed-dose combinations: Already common in hypertension and diabetes, fixed-dose LUTS therapies improve adherence and convenience. Dutasteride–tamsulosin combinations exemplify this trend.
- Novel mechanisms: Beta-3 agonists, potassium channel modulators, and regenerative therapies may soon join the LUTS armamentarium, potentially creating new synergies.
- Precision medicine: Biomarker-driven selection, based on genetics, prostate volume, and urodynamics, could refine which men benefit most from each combination.
The field is moving away from trial-and-error toward tailored polytherapy, mirroring advances in oncology and cardiology.
Conclusion
Combination therapy has transformed the management of male LUTSs. No longer confined to monotherapy, clinicians now wield a toolkit that addresses multiple pathophysiological pathways simultaneously. Alpha-blockers with 5-ARIs reduce long-term progression. Alpha-blockers with antimuscarinics relieve storage symptoms. PDE5 inhibitors, alone or in combination, bridge the gap between urology and sexual medicine.
The challenge is balance—relieving urinary symptoms without imposing unacceptable side effects, preserving sexual function while curbing progression. In this delicate dance, combination therapy offers flexibility, potency, and personalization.
For the modern urologist, the task is clear: move beyond silos, embrace synergy, and treat LUTSs not as a single disease but as a multifaceted syndrome requiring equally nuanced solutions.
FAQ
1. Is combination therapy always better than monotherapy for LUTSs?
Not necessarily. Combination therapy offers superior outcomes in selected patients, especially those with large prostates, severe symptoms, or concomitant erectile dysfunction. But it also carries higher risks of adverse effects, requiring careful patient selection.
2. Are PDE5 inhibitors safe to use with alpha-blockers?
Yes, but with caution. When properly dosed, the risk of hypotension is low. Long-acting selective agents (e.g., tadalafil with tamsulosin) are preferred over short-acting, non-selective combinations.
3. Which patients benefit most from alpha-blocker plus 5-ARI therapy?
Men with large prostates (>40 mL), elevated PSA, and high risk of progression derive the greatest benefit. This combination reduces both acute urinary retention and need for surgery over time.


