Introduction
Infertility is not merely an adult problem—it often begins in childhood. While most discussions on male infertility revolve around aging, lifestyle, or environmental toxins, the foundation for reproductive capacity is laid long before adulthood. Many congenital or acquired pediatric conditions quietly shape a boy’s future fertility long before he contemplates fatherhood.
In fact, global data show that male factors contribute to 20–70% of infertility cases among couples, a statistic that has remained stubbornly high despite advances in reproductive technology. Assisted reproductive techniques (ART)—in vitro fertilization (IVF), intracytoplasmic sperm injection (ICSI), and sperm retrieval—can overcome many barriers, but they do not address the underlying biological damage. Prevention and early intervention, rather than rescue in adulthood, remain the most effective strategies.
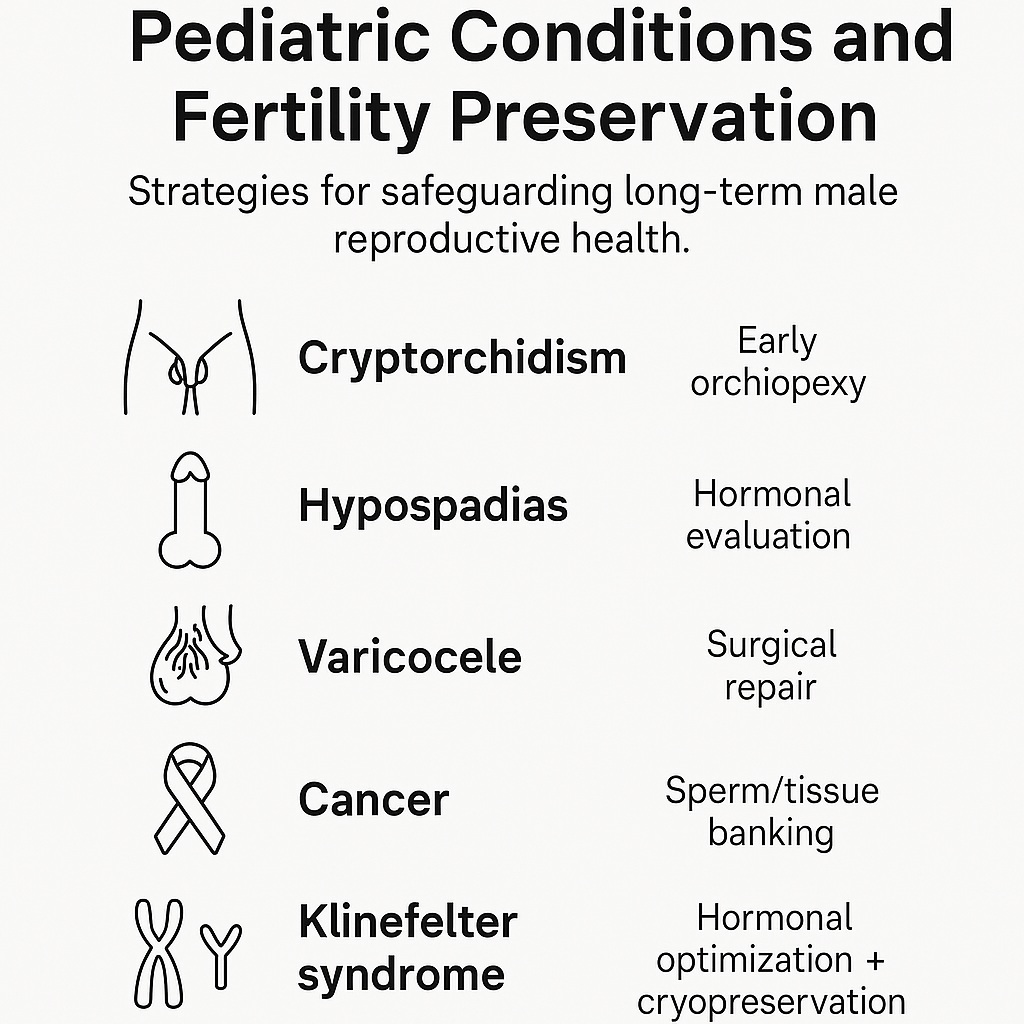
This is the essence of pediatric and adolescent andrology—a field devoted to ensuring that male fertility is preserved from the very beginning. This article explores the major pediatric conditions that can impair testicular function, disrupt hormonal balance, or compromise sexual development, and highlights modern strategies for protecting reproductive potential across a lifetime.
The Undescended Testis: Cryptorchidism and Its Consequences
Cryptorchidism, or undescended testis (UDT), remains the most common developmental disorder of male sexual anatomy, affecting roughly 1–4% of full-term newborns and up to 45% of premature infants. While the condition is often treated for cosmetic or oncologic reasons, its most insidious consequence is impaired spermatogenesis.
The normal descent of the testes into the scrotum ensures an optimal temperature environment for sperm production. In UDT, the elevated temperature of the abdominal cavity or inguinal canal disrupts germ cell maturation, often resulting in a measurable reduction in germ cell density (G/T ratio) and testicular volume. These microscopic changes, seen as early as six months of age, predict poor semen parameters in adulthood.
Timing is everything. Current guidelines from both the American and European Urological Associations recommend orchiopexy between 6 and 18 months of age. Earlier intervention correlates with improved testicular growth, higher inhibin B levels, and better fertility outcomes. Delayed surgery—especially after age 2—has been linked to lower paternity rates and increased use of ART later in life.
Even in unilateral cases, the contralateral “normal” testis may show subclinical damage, perhaps due to shared hormonal or inflammatory mechanisms. Some clinicians are experimenting with gonadotropin therapy (LHRH or hCG) as an adjunct to surgery, aiming to stimulate residual germ cell proliferation. Though promising, these hormonal strategies remain investigational and warrant further study before being adopted in pediatric practice.
Hypospadias: When Form and Function Intertwine
Hypospadias, a condition in which the urethral opening is located on the underside of the penis rather than the tip, affects 0.3–0.8% of male births and appears to be increasing worldwide. While modern reconstructive techniques have improved cosmetic and functional outcomes, fertility impairment often persists, particularly in severe (proximal) cases.
The roots of hypospadias lie in disrupted androgen signaling during fetal development, often reflecting a mild form of testicular dysgenesis. This shared pathway explains why hypospadias frequently coexists with cryptorchidism and other genital anomalies.
Even after surgical correction, affected men may face challenges in adulthood: ejaculatory dysfunction, penile curvature, or altered semen flow patterns. Studies show a 13–21% reduction in fatherhood rates, especially among those with proximal forms of the condition. Subtle hormonal changes—elevated FSH and LH, reduced testosterone—are often present even when semen parameters are normal, indicating partial testicular dysfunction.
The clinical approach should therefore extend beyond cosmetic repair. Evaluation of hormonal profiles, testicular volume, and sexual function is essential in adolescence and adulthood. Addressing residual erectile or ejaculatory dysfunction, when present, can dramatically improve reproductive outcomes and patient confidence.
Surviving Childhood Cancer: Fertility After Chemotherapy and Radiation
Thanks to advances in oncology, over 80% of children diagnosed with cancer now survive into adulthood. Yet these triumphs have created a new challenge—preserving fertility in survivors. Chemotherapeutic agents, particularly alkylating drugs, and radiation exposure can devastate the germinal epithelium, sometimes irreversibly.
Unfortunately, fertility preservation discussions often take a back seat during the chaos of a new cancer diagnosis. Many families, overwhelmed by the immediacy of treatment, defer the topic until it’s too late. However, every pediatric oncologic consultation should now include a fertility preservation plan.
For postpubertal boys, sperm cryopreservation remains the gold standard and can be achieved via masturbation, penile vibratory stimulation, or electroejaculation. For prepubertal patients, experimental protocols involving testicular tissue cryopreservation are under active investigation. Animal studies have shown that cryopreserved testicular grafts can later produce viable sperm—a finding that may soon redefine fertility restoration in pediatric cancer survivors.
Other protective measures include gonadal shielding during radiotherapy and the use of partial orchiectomy instead of total testicular removal when oncologically feasible. These efforts reflect a broader philosophy: survival is not enough; preserving the possibility of future parenthood is equally vital to quality of life.
The Twisting Threat: Testicular Torsion
Testicular torsion, though rare, represents one of the few true surgical emergencies in pediatric urology. If untreated for more than a few hours, ischemia can lead to irreversible testicular necrosis. Even when salvaged, torsed testes may later show impaired spermatogenesis, likely due to oxidative reperfusion injury.
Evidence regarding long-term fertility after torsion is mixed. Some studies report normal paternity and semen parameters, while others note decreased sperm counts and increased oxidative stress markers. Interestingly, men who lose one testis to torsion often maintain near-normal fertility through compensatory hypertrophy of the remaining testis, though psychological effects may persist.
The message is clear: time is tissue. Prompt recognition and surgical detorsion—ideally within 6 hours—remains the single most effective strategy to preserve fertility. Counseling families about the potential reproductive implications is crucial, even in apparently successful cases, to ensure appropriate follow-up and reassurance.
The Adolescent Dilemma: Varicocele and Its Uncertain Legacy
Varicocele, a dilation of the pampiniform plexus veins, affects up to one-third of adolescent boys. While many remain fertile, a subset will experience progressive testicular atrophy, impaired sperm quality, or delayed puberty.
The mechanism is multifactorial—elevated scrotal temperature, venous stasis, oxidative stress, and hormonal disturbances all contribute to germ cell damage. Determining which patients warrant intervention remains controversial.
Current consensus supports varicocelectomy when there is:
- A significant testicular size discrepancy (>20% volume difference)
- Abnormal semen parameters
- Persistent scrotal pain
Surgical or embolization repair in adolescence has shown durable improvements in testicular growth and sperm quality, suggesting that early correction may prevent lifelong reproductive deficits. Nevertheless, overdiagnosis must be avoided; not every varicocele demands repair, and careful selection based on objective criteria is key.
Infections and Inflammation: The Hidden Saboteurs
While less common in childhood, epididymo-orchitis and viral orchitis (particularly mumps) can cause lasting damage to the seminiferous tubules. The acute infection may resolve, but scarring or obstruction of the efferent ducts can result in obstructive azoospermia years later.
Prompt antibiotic therapy and supportive care are essential to prevent chronic inflammation and fibrosis. In cases where obstruction occurs, microsurgical reconstruction of the vas deferens or sperm retrieval for IVF may restore fertility.
Equally important is vaccination—the resurgence of mumps in under-immunized populations has reignited concern about post-mumps infertility. Thus, public health measures intersect directly with reproductive medicine in safeguarding future male fertility.
The Neurologic Factor: Spina Bifida and Ejaculatory Dysfunction
Spina bifida, a congenital defect of the spinal cord, has evolved from a lethal disorder to a chronic condition compatible with long-term survival. As more affected boys reach adulthood, issues of sexual and reproductive function have become increasingly relevant.
Infertility in spina bifida arises from two primary mechanisms: defective spermatogenesis and ejaculatory failure. Even when sperm are present, semen parameters are often suboptimal. Advances in reproductive technology, however, have dramatically improved outcomes. Techniques such as penile vibratory stimulation, electroejaculation, and ICSI now allow many of these men to father biological children.
Erectile dysfunction, reported in up to 75% of cases, can often be effectively treated with sildenafil or other PDE5 inhibitors, enhancing not only fertility but also psychological well-being. The challenge lies in continuity of care—fertility is rarely discussed during the transition from pediatric to adult urology. Early counseling and sexual health education should become routine for adolescents with neurologic conditions, ensuring that fertility is part of lifelong care planning.
Genetic Syndromes and Endocrine Disorders: Hidden Codes of Infertility
A substantial fraction of male infertility cases have genetic origins, often identifiable in childhood. Among these, Klinefelter syndrome (47,XXY) and congenital adrenal hyperplasia (CAH) stand out as critical models of endocrine disruption.
Klinefelter Syndrome
Klinefelter syndrome (KS) is the most common chromosomal cause of nonobstructive azoospermia. The classic phenotype includes small, firm testes, tall stature, gynecomastia, and hypogonadism. However, many cases remain undiagnosed until adulthood, discovered during infertility evaluation.
Early hormonal intervention can improve outcomes. Adolescents with KS should undergo semen analysis and hormone profiling. If sperm are found, immediate cryopreservation is recommended, as germ cell depletion progresses rapidly after puberty. Gonadotropin-based therapies—using clomiphene, aromatase inhibitors, or hCG—can enhance intratesticular testosterone and improve sperm retrieval rates during micro-TESE. Early diagnosis, therefore, transforms a once-inevitable infertility into a manageable condition.
Congenital Adrenal Hyperplasia
CAH results from enzymatic defects in cortisol synthesis, most commonly 21-hydroxylase deficiency, leading to androgen excess and, paradoxically, gonadal dysfunction. High ACTH levels promote the growth of testicular adrenal rest tumors (TARTs)—benign but space-occupying lesions that compress seminiferous tubules.
Regular testicular ultrasound from early childhood and optimized steroid replacement therapy are the cornerstones of prevention. Effective hormonal control suppresses ACTH, stabilizes testicular architecture, and preserves spermatogenesis. In severe cases, surgical sperm retrieval may still be possible, but prevention remains preferable to intervention.
From Pediatric Urology to Reproductive Medicine: The Imperative of Continuity
The thread connecting all these conditions is timing—the earlier the diagnosis and intervention, the greater the chance of preserving fertility. Yet, pediatric and adult care often exist in silos, with little communication during the transition years.
Adolescent and young adult males, especially those with chronic illnesses or developmental anomalies, must not “fall through the cracks.” Structured transition-of-care programs are essential to maintain surveillance, counsel patients, and discuss reproductive goals early and openly.
As the field evolves, experimental frontiers—such as testicular tissue cryopreservation, stem-cell-derived spermatogenesis, and gonadotropin modulation—offer exciting possibilities. These innovations, once refined, may finally bridge the decades-long gap between childhood disease and adult fertility outcomes.
Conclusion
The journey to male fertility begins not in the bedroom, but in the nursery. The conditions that shape a man’s reproductive potential often emerge in infancy or childhood—sometimes silently, sometimes dramatically. Whether through timely orchiopexy, hormonal therapy, varicocele repair, or sperm banking, early recognition and proactive care can transform lifelong outcomes.
The next generation of pediatric and reproductive specialists must think beyond immediate survival or cosmetic outcomes and embrace fertility preservation as a core component of pediatric medicine. To ignore fertility in childhood care is to rob adulthood of one of its most profound experiences: the ability to create life.
FAQ: Pediatric Fertility and Long-Term Male Reproductive Health
1. Can childhood surgery for undescended testis completely restore fertility?
Early orchiopexy—ideally before 18 months—significantly improves fertility potential, but may not fully normalize it, especially in bilateral cases. The earlier the intervention, the better the germ cell preservation.
2. How can fertility be protected in boys undergoing cancer treatment?
Postpubertal patients should bank sperm before therapy. For younger boys, experimental testicular tissue cryopreservation is available at select centers. Gonadal shielding during radiation is also critical.
3. Should boys with Klinefelter syndrome attempt sperm preservation during adolescence?
Yes. Early semen analysis and cryopreservation are recommended once sperm are detectable, as spermatogenesis often declines rapidly after puberty.