Introduction: Two Old Drugs, One Persistent Problem
Pulmonary arterial hypertension (PAH) remains one of the most devastating chronic cardiovascular disorders, characterized by elevated pulmonary artery pressure, progressive vascular remodeling, and eventual right heart failure. Despite the availability of several pharmacological classes — endothelin receptor antagonists, phosphodiesterase type-5 inhibitors, and prostacyclin analogues — the disease continues to carry a heavy clinical burden and high mortality rates.
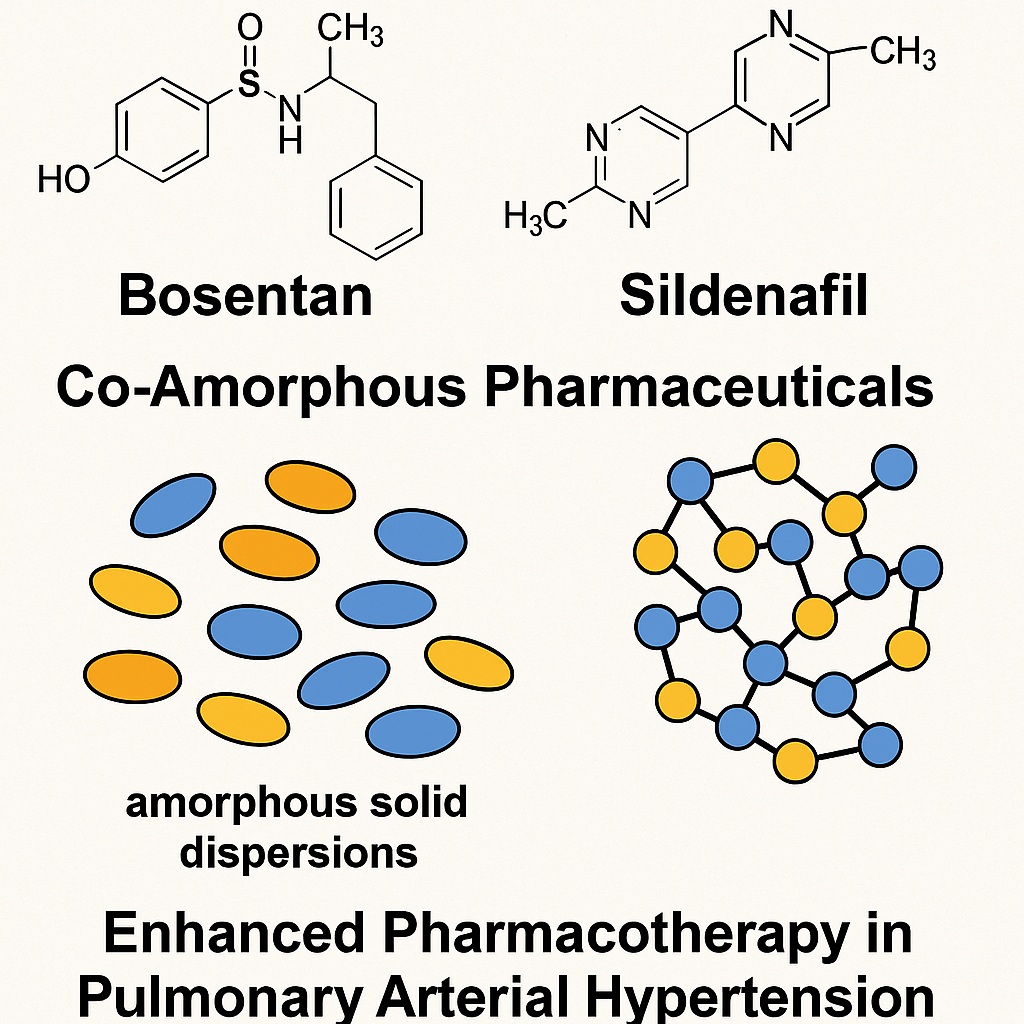
Bosentan and sildenafil represent two pillars of PAH management, each targeting distinct yet complementary signaling pathways. Bosentan, a dual endothelin receptor antagonist, mitigates vasoconstriction and vascular proliferation, while sildenafil, a phosphodiesterase type-5 (PDE5) inhibitor, enhances nitric oxide–mediated vasodilation by preventing cGMP degradation. When used in combination, they synergistically address multiple pathogenic mechanisms of PAH, improving hemodynamics, exercise capacity, and time to clinical worsening.
However, both drugs share a major pharmacotechnical obstacle: poor aqueous solubility and limited oral bioavailability (approximately 41–50%). Bosentan’s acidic nature and sildenafil’s basic properties cause strong pH-dependent solubility variations, resulting in incomplete absorption and erratic pharmacokinetics. This fundamental limitation has long restricted the development of efficient fixed-dose combinations — an increasingly valuable approach in chronic cardiovascular therapy.
The recent work by Strojewski et al. (2024) explores an innovative route to overcome these barriers. By co-amorphizing bosentan monohydrate and sildenafil base through high-energy ball milling, the researchers investigated whether mechanical activation could yield a molecularly homogeneous amorphous system with improved dissolution, supersaturation, and stability. This study does more than describe a formulation technique — it represents a conceptual shift toward pairing weak acids and weak bases in solid-state molecular alloys to achieve enhanced drug performance.
Rationale for Co-Amorphization: When Opposites Attract
The hypothesis driving this investigation stems from a simple chemical truth: bosentan and sildenafil are opposites in acid-base character. Bosentan monohydrate, a weak acid (pKa ≈ 5.46), dissolves better at neutral or basic pH, while sildenafil base (pKa ≈ 5.99) shows the reverse, with high solubility under acidic gastric conditions but sharp decline at intestinal pH.
By co-processing these two molecules, the researchers anticipated that proton-transfer interactions and hydrogen bonding could stabilize a single amorphous phase. Such co-amorphous drug–drug systems often display enhanced solubility and dissolution due to disruption of crystalline lattices and formation of molecularly dispersed phases. The intimate mixing at the atomic level prevents re-crystallization, supports higher free-energy states, and allows the generation of supersaturated solutions capable of improving bioavailability.
This approach also aligns with the clinical logic of PAH treatment: combining drugs that act synergistically in vivo should, ideally, coexist synergistically in vitro. If successful, such co-amorphization could serve as a technological foundation for next-generation fixed-dose combination products, streamlining patient compliance and therapeutic control.
Methods in Motion: The Mechanics of Molecular Transformation
The study employed high-energy ball milling, a mechanochemical process known for inducing solid-state transformations without solvents. Binary mixtures of bosentan and sildenafil, in varying weight ratios (BOS fractions of 0.2, 0.5, 0.8), were milled in zirconium oxide jars at 400 rpm for four hours, with intermittent pauses to prevent overheating.
This intense mechanical activation promotes particle fracture, plastic deformation, and local temperature rises, leading to amorphization of crystalline structures. The products were then evaluated using an impressive array of analytical tools, each probing a different dimension of the new solid forms:
- Powder X-ray diffraction (XRD) confirmed the disappearance of sharp crystalline peaks, replaced by broad halos typical of amorphous systems.
- Differential scanning calorimetry (DSC) provided evidence of single glass transitions (Tg = 64–78 °C), indicating molecularly homogeneous amorphous phases rather than mere physical mixtures.
- Fourier-transform mid-infrared spectroscopy (FT-MIR) detected band broadening — a fingerprint of structural disorder — but no new covalent bonds, implying non-destructive intermolecular interactions.
- Dielectric spectroscopy and polarizing optical microscopy revealed how these amorphous systems behaved under thermal stress, highlighting their stability and crystallization dynamics.
- Finally, HPLC-DAD quantification established precise dissolution and supersaturation profiles in simulated gastric and intestinal environments.
Such methodological thoroughness illustrates the increasing sophistication of modern pharmaceutics: the boundary between chemistry and physics has blurred, giving rise to the discipline of mechanochemistry — chemistry without solvents, but not without drama.
Crystalline to Amorphous: The Dance of Disorder
One of the most striking observations in this work was the complete disappearance of crystalline order in co-milled samples. Both bosentan and sildenafil, when processed separately, are stable crystalline solids with monoclinic symmetry. Yet, after co-milling, their XRD diffractograms lost all signature peaks, replaced by smooth amorphous halos.
DSC thermograms corroborated these findings. Physical mixtures displayed distinct melting endotherms corresponding to each drug, but amorphous dispersions showed a single glass transition — clear proof of molecular miscibility. Interestingly, the position of the Tg increased with bosentan content, reflecting its higher glass-forming ability and thermal stability. Formulations containing 50–80 wt % bosentan (BM0.5 and BM0.8) demonstrated the greatest resistance to recrystallization upon heating up to 190 °C.
These results indicate that bosentan acts as a stabilizing matrix for sildenafil molecules, suppressing their tendency to revert to a crystalline form. The Gordon-Taylor equation fitting confirmed near-ideal mixing behavior, with experimental data closely matching the predicted Tg curve. Such thermodynamic harmony is rare among binary drug systems, where mismatched molecular sizes or incompatible polarities often cause phase separation.
Stability and Fragility: The Dual Personality of Amorphous Solids
Amorphous systems are, by definition, metastable. They offer enhanced solubility and dissolution but are prone to recrystallization, especially under stress conditions of heat and humidity. Strojewski et al. approached this dilemma with rigorous physical characterization.
Using frequency-domain dielectric spectroscopy, the researchers examined molecular relaxation processes — microscopic motions that underpin macroscopic stability. Two types were identified:
- α-relaxation, associated with the dynamic glass transition and cooperative molecular mobility, and
- β-relaxation, reflecting localized reorientations within the amorphous matrix.
The presence of bosentan was found to slow down molecular mobility, reducing the rate of β-relaxation and effectively stabilizing sildenafil molecules within the amorphous phase. The calculated fragility index (mp ≈ 120) classified the binary dispersion as a “fragile” glass former — one that undergoes rapid dynamic changes near its Tg — yet still exhibited sufficient thermal resilience under ambient conditions.
Moreover, after two weeks of storage under accelerated conditions (40 °C/75 % RH), the co-amorphous formulations remained largely amorphous, showing only minimal recrystallization traces. This demonstrates that a well-balanced molecular interaction between the acid and base components can yield a practically stable amorphous drug–drug alloy.
Surface Science: Particle Size, Wettability, and the Hydrophilic Turn
High-energy milling not only transforms molecular structure but also reshapes particles themselves. The process drastically reduced the mean particle size (d50) of both drugs — from 209 μm for bosentan and 23 μm for sildenafil to approximately 7–14 μm in co-milled dispersions. Smaller particles mean larger surface area, which in turn accelerates dissolution and wetting.
Contact-angle measurements revealed another favorable outcome: increased surface hydrophilicity. The mean contact angle decreased by about ten degrees compared with the crystalline forms, indicating that the amorphous surfaces interact more readily with water. This is consistent with the hypothesis that amorphization exposes polar functional groups previously locked within crystal lattices, thus enhancing hydrogen bonding with solvent molecules.
These physical changes — finer particles, smoother surfaces, and improved wettability — collectively amplify the dissolution rate, complementing the intrinsic thermodynamic advantages of the amorphous state.
Dissolution Dynamics: Supersaturation and Beyond
The ultimate test of a new solid-state form lies in its dissolution behavior. In this study, dissolution profiles were recorded in simulated gastric fluid (pH 1.2) and phosphate buffer (pH 6.8) to mimic in vivo transitions from stomach to intestine.
As expected, sildenafil dissolved rapidly in acidic medium, achieving immediate and complete release under sink conditions, while bosentan remained below detection due to its poor solubility at low pH. However, in intestinal conditions — where bosentan ionizes and sildenafil’s solubility plummets — the co-amorphous dispersions displayed remarkable performance.
Formulations with 20–50 wt % sildenafil (BM0.5 and BM0.8) produced long-lasting bosentan supersaturation in phosphate buffer, with concentrations significantly exceeding the crystalline solubility limit. This supersaturation persisted over time, suggesting that the amorphous phase not only facilitated rapid release but also stabilized the dissolved state against precipitation.
In contrast, samples rich in sildenafil (BM0.2) failed to sustain supersaturation, highlighting the delicate balance required for optimal drug ratio. Bosentan, once again, emerged as the stabilizing hero — its higher Tg and hydrogen-bonding potential anchoring the amorphous matrix and suppressing sildenafil’s crystallization drive.
These findings demonstrate that co-amorphization can achieve what formulation scientists long strive for: sustained supersaturation, the key to improved oral absorption of poorly soluble drugs.
Mechanistic Insights: A Molecular Partnership
What makes bosentan and sildenafil such compatible partners? The answer lies in complementary molecular features. Bosentan’s sulfonamide and pyrimidine groups serve as hydrogen-bond donors and acceptors, while sildenafil’s pyrazolopyrimidinone and piperazine rings provide multiple sites for interaction.
During high-energy milling, these molecules likely form reversible hydrogen-bond networks and electrostatic associations, producing a molecularly dispersed phase. FT-MIR analysis confirmed broadening of characteristic bands — evidence of structural disorder — yet no new peaks, confirming that the process does not induce chemical degradation or salt formation.
The resulting material behaves as a molecular alloy, where the individual identities of the drugs blur into a cooperative solid solution. Such “alloyed pharmaceuticals” are an emerging frontier in drug design, allowing developers to engineer physical properties without altering chemical composition — a far more efficient and regulatory-friendly strategy than synthesizing new salts or cocrystals.
Therapeutic Implications: Toward Smarter Combinations
From a pharmacotherapeutic standpoint, the implications of this study extend far beyond bosentan and sildenafil themselves. Co-amorphization offers a template for the rational design of fixed-dose combinations in chronic diseases where polypharmacy is standard practice.
In PAH, combining an endothelin receptor antagonist with a PDE5 inhibitor is already an established clinical approach. Translating this synergy into a single amorphous formulation could enhance bioavailability, simplify dosing, and improve patient adherence — all without the need for complex excipients or polymer carriers.
Moreover, the observed physical stability of the co-amorphous system suggests potential feasibility for scale-up and industrial manufacturing. High-energy milling is a solvent-free, environmentally benign, and cost-effective process — attributes that align well with modern pharmaceutical sustainability goals.
Beyond PAH, this strategy could inspire similar formulations across therapeutic areas where multiple poorly soluble drugs must coexist: oncology, infectious diseases, or neurodegenerative disorders. The concept of molecularly matched drug pairs — selected for complementary solubility, pKa, or hydrogen-bonding characteristics — may well represent the next generation of oral solid dosage design.
A Glimpse into the Future: Mechanochemistry Meets Medicine
The findings by Strojewski et al. exemplify a broader shift in pharmaceutical science — from passive formulation to active solid-state engineering. Where once the crystal was king, today the amorphous form reigns, albeit precariously.
Mechanochemistry, once regarded as an academic curiosity, has emerged as a mainstream tool for creating complex materials with precise physical attributes. Its application to drug–drug systems, as demonstrated here, heralds a new era of rational, eco-friendly formulation science.
In this context, bosentan and sildenafil serve as model citizens — not merely for their therapeutic synergy but for their cooperative behavior at the molecular level. Their union illustrates how understanding solid-state chemistry can translate directly into clinical benefit, bridging the gap between the lab bench and the patient’s bedside.
Conclusion: Two Companions in Science and Therapy
In summary, the co-amorphization of bosentan monohydrate and sildenafil base through high-energy ball milling successfully produced homogeneous, thermally stable molecular alloys with enhanced dissolution and supersaturation characteristics. The process harnesses the natural acid–base complementarity of the two drugs to overcome their individual solubility limitations, offering a promising path toward a fixed-dose combination therapy for pulmonary arterial hypertension.
This work not only advances formulation technology but also illustrates a philosophical point: sometimes, the most effective partnerships in medicine begin at the molecular level. When two compounds cooperate in the solid state as harmoniously as they do in the bloodstream, science takes a decisive step toward more intelligent, integrated therapeutics.
Frequently Asked Questions (FAQ)
1. Why are bosentan and sildenafil often combined in pulmonary arterial hypertension therapy?
Because they act on different yet complementary biological pathways. Bosentan blocks endothelin-mediated vasoconstriction, while sildenafil enhances nitric oxide–driven vasodilation. Together, they reduce pulmonary pressure more effectively than either drug alone.
2. What advantages does the co-amorphous form offer over traditional formulations?
Co-amorphous systems improve solubility, dissolution rate, and the ability to maintain supersaturation in gastrointestinal fluids. This leads to higher and more consistent bioavailability without chemical modification or polymer additives.
3. Is high-energy ball milling suitable for industrial production of such formulations?
Yes. The technique is solvent-free, scalable, and relatively simple to control. However, further studies on long-term stability, manufacturability, and in vivo bioequivalence are needed before clinical application.