Sustained progress in reproductive medicine increasingly depends on drug-delivery systems capable not only of releasing therapeutic agents effectively, but also of delivering them precisely to the tissues where they provide the greatest benefit. Among women experiencing recurrent pregnancy loss, thin endometrium, impaired uterine blood flow, or inadequate tissue responsiveness, sildenafil citrate has emerged as a surprisingly powerful pharmacological ally. What began as a cardiovascular drug and rose to fame through its well-known urologic application now occupies a meaningful place in reproductive science. Yet its full therapeutic potential has remained constrained by an obstacle both mundane and stubborn: the absence of an effective, well-designed vaginal dosage form.
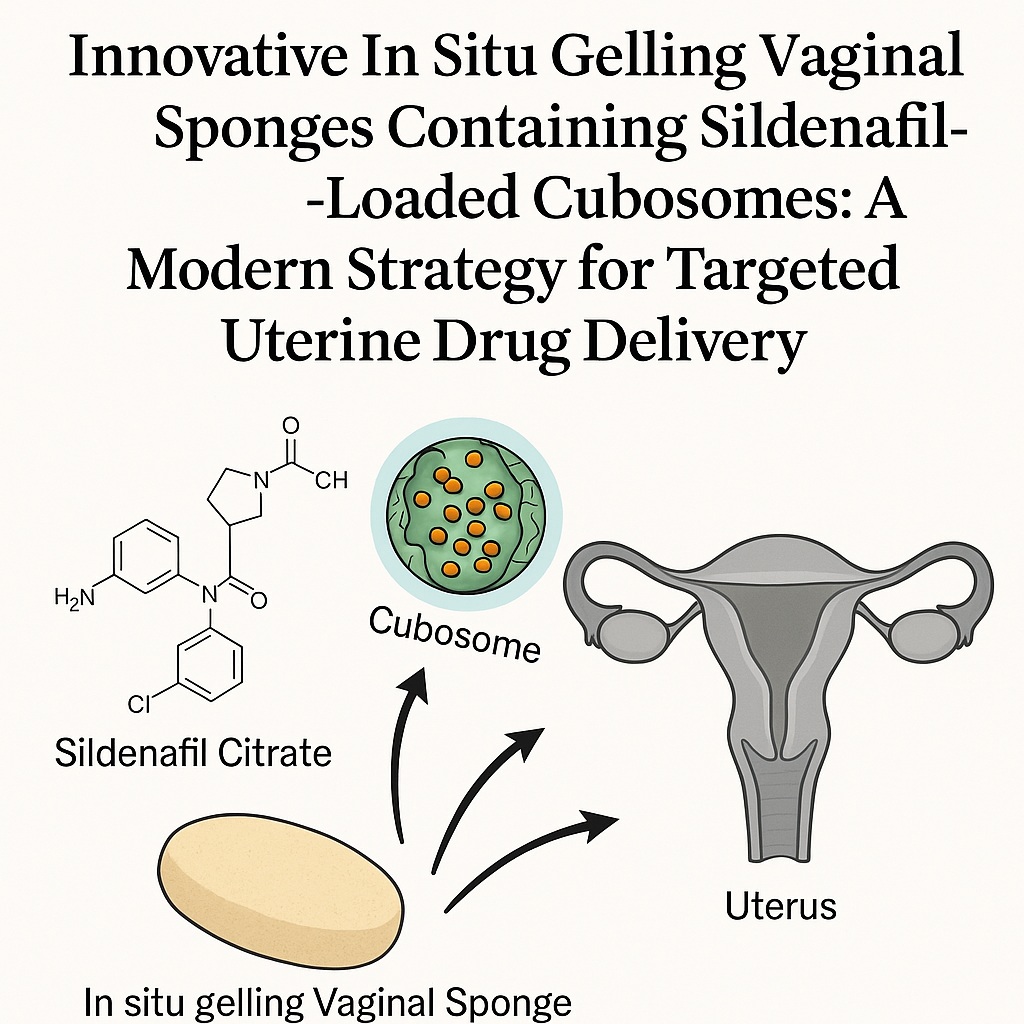
A recent experimental study addressed this gap through a sophisticated formulation strategy—sildenafil citrate–loaded cubosomes embedded within in situ gelling vaginal sponges. The approach melds nanotechnology, mucoadhesive systems, chitosan-based gelation, and controlled drug release into a single delivery platform intentionally engineered for efficient uterine targeting with minimal systemic exposure . The result is a compelling pharmaceutical system that enhances local bioavailability, avoids the adverse effects of oral sildenafil, and improves the uterine response essential for successful implantation.
This article provides an extensive, readable, and medically rigorous exploration of this innovative drug-delivery design: how it works, why it matters, and what distinguishes it from existing therapies.
Reproductive Challenges and the Rationale for Targeted Sildenafil Delivery
Repeated pregnancy loss remains one of the most disheartening reproductive complications, burdening 2–5% of couples worldwide. Despite advances in assisted reproductive technologies, the relationship between endometrial thickness, uterine blood flow, and implantation success continues to dominate treatment decisions. A well-vascularized, receptive endometrial lining—typically exceeding 8 mm—correlates strongly with successful embryo implantation and ongoing pregnancy. When this lining is too thin or insufficiently perfused, the chances of conception inevitably diminish.
Sildenafil citrate offers a biologically elegant solution. As a type-5 phosphodiesterase inhibitor, it increases nitric-oxide–mediated vasodilation and thereby enhances blood flow to the uterine lining. Multiple clinical observations have documented its positive impact on endometrial proliferation and uterine hemodynamics when delivered intravaginally. However, the practical challenges are considerable. Oral sildenafil produces:
- pronounced systemic adverse effects such as headaches, flushing, and hypotension,
- suboptimal uterine tissue concentrations, and
- poor therapeutic consistency across patients.
Moreover, because no approved vaginal dosage form previously existed, investigators relied on crushed oral tablets introduced vaginally—an approach both inelegant and ineffective due to rapid dissolution, poor mucoadhesion, and fast clearance by vaginal fluids.
The vaginal environment itself creates additional hurdles. With a naturally acidic pH (3.5–4.5), high fluid turnover, and relatively low permeability for hydrophilic drugs, it is an inhospitable site for maintaining therapeutic levels of conventional formulations. Thus emerged the need for a new system—one that would overcome rapid clearance, allow sustained release, and dramatically increase drug residency at the uterine interface.
Cubosomes, with their unique lipid-based nanostructure, offered the first part of the solution. In situ gelling sponges supplied the second.
Cubosomes as a Modern Nanocarrier for Vaginal Drug Delivery
Cubosomes represent one of nanotechnology’s more fascinating contributions to pharmacy: self-assembled lipid particles exhibiting a highly ordered yet dynamic bicontinuous cubic crystalline phase. In the study, the particles were prepared using glyceryl monooleate (GMO) as the lipid and poloxamer 407 as the surfactant, with optional incorporation of polyvinyl alcohol (PVA) for additional stabilization .
Structural Advantages of Cubosomes
Their internal architecture—composed of two continuous, intertwined aqueous channels separated by a lipid bilayer—results in:
- high drug-loading capacity for both hydrophilic and lipophilic molecules,
- sustained drug release due to restricted diffusion pathways,
- excellent biodegradability owing to the enzymatic breakdown of monooleate lipids, and
- strong mucoadhesive interactions through hydrogen bonding and surface association.
These attributes render cubosomes ideal for targeting mucosal surfaces and delivering drugs over extended intervals without the burst-and-washout pattern typical of gels and suppositories.
Optimization of Sildenafil-Loaded Cubosomes
The study employed a 4² factorial design, adjusting concentrations of poloxamer 407 and PVA to identify an optimized formulation with the smallest particle size, highest drug-entrapment efficiency, and controlled release profile. Entrapment efficiencies ranged from 32% to 72%, and particle sizes from 150 to 446 nm—squarely within the nanometric range conducive to mucosal penetration and stable dispersion.
Poloxamer concentration exerted a dual influence. Increasing it up to a threshold reduced particle size and improved stabilization; exceeding that threshold disrupted structural organization and enlarged the particles. PVA acted similarly: moderate concentrations enhanced stability, while excessive amounts increased viscosity and hindered proper emulsification.
Release kinetics across formulations reflected diffusion-controlled, non-Fickian transport, consistent with the complex lipid bilayer network of GMO-based cubosomes.
Ultimately, the optimized formulation—containing approximately 11% poloxamer 407 and 3% PVA—exhibited the most desirable characteristics for vaginal application and drug retention .
From Nanoparticles to Sponges: The Innovation of In Situ Vaginal Gelation
A nanocarrier, however sophisticated, cannot overcome the vaginal clearance mechanism alone. Gravity and fluid turnover work persistently to remove externally applied formulations within hours. To solve this, researchers incorporated the optimized cubosomal dispersion into in situ gelling chitosan-based vaginal sponges—small, freeze-dried inserts that hydrate upon administration and convert into a cohesive, mucoadhesive gel.
Why Chitosan?
Chitosan, a cationic polysaccharide derived from chitin, is widely recognized for:
- exceptional mucoadhesive strength through electrostatic interactions with negatively charged mucins,
- pH-responsive gelation, particularly strong at acidic vaginal pH,
- ability to enhance paracellular permeability, and
- biocompatibility and biodegradability.
In this design, chitosan at 2% w/w provided the most balanced profile: adequate hardness for handling, strong mucoadhesion, and sustained release without excessive rigidity.
When inserted, each sponge swiftly absorbed vaginal fluid, swelling into a robust yet comfortable gel that held the cubosomes in intimate contact with mucosal tissue for many hours. This greatly extended the formulation’s residence time—one of the central goals of the system.
Histopathological Confirmation of Enhanced Uterine Targeting
A crucial portion of the investigation involved in vivo studies in female Wistar rats, comparing intravaginal CIS (cubosomal in situ sponges) with free sildenafil sponges and oral sildenafil solution.
The findings were striking. Uterine samples from rats receiving intravaginal cubosomal sponges showed:
- a massive increase in endometrial epithelial thickness,
- expansion of endometrial glands,
- marked rise in vascularity and angiogenesis, and
- increased blood-vessel caliber within both uterus and ovary.
These effects were significantly greater than those observed with free sildenafil sponges and dramatically more pronounced than after oral administration.
The endometrial thickness increased from approximately 1014 μm in controls to 1382 μm in CIS-treated rats—a physiologically meaningful enhancement associated with improved implantation potential .
Tissue staining (H&E and PAS) clearly supported enhanced glandular activity and improved vascular perfusion. Importantly, no pathological signs of irritation were reported, attesting to the formulation’s local tolerability.
Pharmacokinetic Behavior: Lower Systemic Levels, Higher Local Impact
If the histological findings demonstrated the formulation’s effectiveness, the pharmacokinetic profile explained why. Compared to oral sildenafil, intravaginal CIS produced:
- dramatically lower Cmax and plasma exposure,
- prolonged half-life, and
- delayed Tmax reflecting gradual mucosal absorption.
For example, oral sildenafil achieved a Cmax of over 1280 ng/mL, while intravaginal CIS produced only 134 ng/mL—a nearly ten-fold reduction in systemic concentration. Yet local uterine effects were amplified rather than diminished.
This discrepancy supports the mechanism known as the first uterine pass effect: drugs delivered intravaginally may traverse local venous networks that countercurrently transfer molecules directly to the uterus before reaching systemic circulation.
Thus, intravaginal CIS achieved precisely what the researchers intended:
high local pharmacodynamic activity with minimized systemic burden.
This balance is especially valuable in reproductive medicine, where minimizing systemic exposure reduces risks such as hypotension and headache—common adverse effects of oral sildenafil therapy.
Broader Implications and Future Potential
Taken together, these findings demonstrate a formulation approach that elegantly bridges nanotechnology, mucosal pharmacokinetics, bioadhesion, and reproductive physiology. The vaginal cubosomal sponge system offers:
- improved drug stability and tissue permeability,
- sustained local release without dosing frequency burdens,
- reduced systemic toxicity, and
- enhanced endometrial receptivity—a key requirement for implantation.
Although further studies—particularly biodistribution in human tissues—are necessary, this work establishes a strong theoretical and experimental foundation for future clinical translation.
The implications extend beyond sildenafil. Any therapeutic agent intended for uterine action—hormones, vasodilators, anti-inflammatory compounds, or gene-modifying molecules—may benefit from similar delivery systems.
FAQ
1. Why is intravaginal delivery superior to oral sildenafil for reproductive indications?
Intravaginal delivery avoids extensive first-pass metabolism, minimizes systemic exposure, and utilizes the first uterine pass effect, allowing higher local concentrations at the endometrium. This results in improved vascularity and endometrial thickness without the adverse systemic effects of oral sildenafil.
2. What makes cubosomes particularly suitable for vaginal drug delivery?
Cubosomes combine high surface area, strong mucoadhesion, controlled release properties, and the ability to encapsulate different drug types. Their lipidic bilayer structure mimics biological membranes, allowing enhanced permeation and stable retention at mucosal sites.
3. Do in situ gelling sponges offer advantages over conventional gels or tablets?
Yes. Sponges hydrate into a gel that adheres firmly to the vaginal mucosa, resists rapid clearance, releases drug slowly, and provides precise dosing. This structure significantly prolongs drug residence time and improves therapeutic performance compared to gels, suppositories, or crushed tablets.