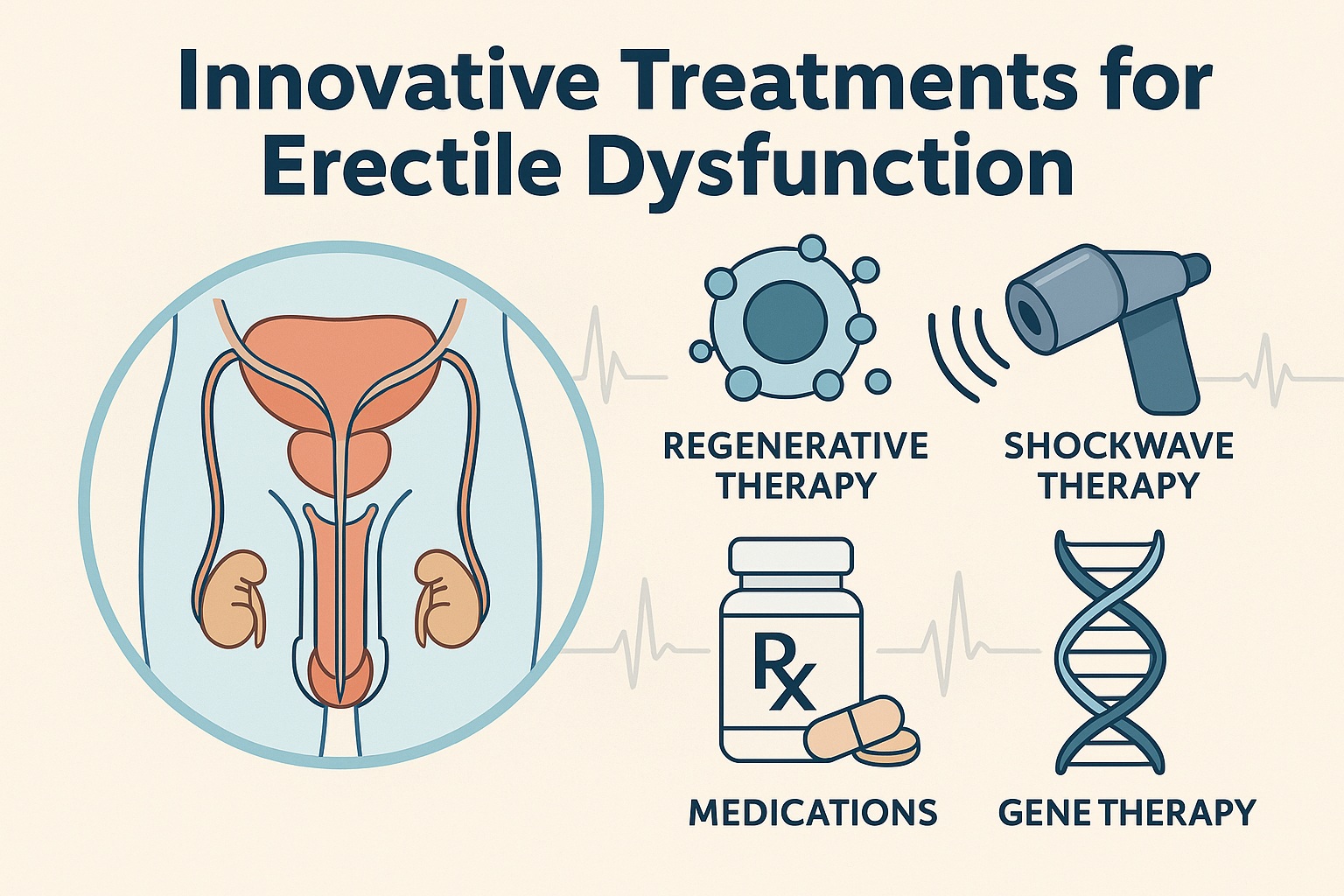
Erectile dysfunction (ED) is far more than a clinical diagnosis confined to pharmacological management; it is a complex interplay of vascular, neurological, hormonal, psychological, and relational factors. While phosphodiesterase type 5 inhibitors (PDE5Is) transformed the therapeutic landscape more than two decades ago, modern research makes one point abundantly clear: the future of ED therapy will not be defined by a single class of drugs. Instead, it is evolving toward multimodal, regenerative, device-based, and even gene-oriented approaches—all aimed at addressing the underlying pathophysiology rather than simply managing symptoms.
The systematic review underpinning this article presents a sweeping overview of the innovative treatments that may soon redefine ED care. In this fully re-imagined narrative, the goal is to synthesize the evidence, contextualize emerging approaches, and illustrate how treatment paradigms are shifting toward precision medicine. The tone is serious and professional, but not without moments of dry academic humor—after all, sexual medicine has always required a delicate balance of rigor and humanity.
Redefining ED Management: Why Innovation Is Necessary
The dominance of PDE5 inhibitors in the ED arena is well earned, but not absolute. Despite their effectiveness, a considerable proportion of men—particularly those with diabetes, severe vascular disease, post-surgical changes, or advanced age—do not respond adequately. For these patients, therapeutic innovation is not simply welcome; it is necessary.
Moreover, modern patients increasingly seek treatments that:
- address root causes
- restore physiological erectile function
- require minimal preparation
- offer durable results rather than episodic symptom relief
This shift in expectations parallels broader trends in medicine, particularly the transition toward tissue regeneration and personalized therapeutics. As clinicians confront a growing population of men dissatisfied with traditional therapies, the exploration of alternatives becomes more than academic curiosity.
Finally, innovation is driven by a deeper understanding of ED pathogenesis. Research continues to illuminate the molecular and vascular mechanisms responsible for compromised penile hemodynamics. Merely augmenting nitric oxide signaling—essentially the entire job description of PDE5Is—cannot fully address endothelial dysfunction, fibrosis, or neurovascular injury.
Thus, modern approaches aim higher: restoring tissue integrity, reversing pathological remodeling, and enhancing neurovascular regeneration.
Regenerative Medicine: The New Frontier of ED Treatment
Regenerative medicine has become the most captivating area of ED research. The belief that erectile tissue can be repaired—or at least functionally improved—represents a paradigm shift from symptomatic treatment to true disease modification.
Stem Cell Therapy
Stem cell interventions hold tremendous promise because they target the underlying vascular and neural deficits characteristic of ED. Experimental and early clinical studies demonstrate that mesenchymal stem cells (MSCs), adipose-derived stem cells (ADSCs), and bone marrow–derived progenitors all possess the capacity to:
- stimulate angiogenesis
- reduce fibrosis
- restore smooth muscle integrity
These effects collectively improve cavernosal hemodynamics, offering hope for patients whose conditions extend beyond the reach of PDE5 inhibitors. While the majority of studies remain preclinical, phase I and II trials report safety and encouraging efficacy signals. Importantly, stem cells do not appear to differentiate into penile tissue per se; their benefits arise mainly from paracrine effects—essentially acting as biochemical “coaches” for injured tissue.
The challenge lies in standardizing cell isolation, dosing, delivery routes, and long-term safety monitoring. But the trajectory of the data is promising enough that stem cell therapy is likely to become a mainstream option, assuming regulatory hurdles can be addressed.
Platelet-Rich Plasma (PRP)
Platelet-rich plasma, long popular in sports medicine, has entered sexual medicine with surprising momentum. PRP delivers concentrated growth factors directly into the penile tissues, promoting vascular regeneration and reducing inflammation. While anecdotal enthusiasm sometimes outpaces scientific rigor, controlled trials demonstrate modest but real improvements in erectile function scores.
Unlike stem cells, PRP is autologous, simple to prepare, and relatively inexpensive. However, variability in preparation protocols complicates interpretation across studies. Standardization remains essential before PRP can be endorsed confidently as an evidence-based ED therapy.
Gene Therapy
Once considered a distant dream, gene therapy is emerging as a plausible option for severe or refractory ED. Initial experiments have focused on upregulating genes that enhance nitric oxide signaling, improve smooth muscle function, or modulate ion channel activity.
Gene therapy offers the tantalizing possibility of sustained benefit with a single intervention. But safety concerns, regulatory complexity, and ethical considerations temper enthusiasm. Despite these challenges, early trials demonstrate that certain vectors are both safe and biologically active, giving hope that gene-based treatments may eventually complement or replace pharmacologic regimens.
Energy-Based Therapies and Device Innovations
Beyond biologics, ED research has expanded significantly into device-based and energy-mediated treatments. These approaches seek to enhance tissue function rather than replace it.
Low-Intensity Extracorporeal Shockwave Therapy (Li-ESWT)
Li-ESWT has quickly become one of the most studied non-pharmacological therapies for ED. The mechanism is subtly elegant: low-intensity mechanical waves induce microtrauma, stimulating angiogenesis, increasing penile blood flow, and upregulating regenerative pathways.
Multiple trials report improved erectile scores, even among PDE5I non-responders. Long-term benefits remain under investigation, but evidence suggests that Li-ESWT may serve as both a standalone treatment and a tool to enhance responsiveness to pharmacotherapy.
Challenges remain regarding:
- optimal energy levels
- treatment frequency
- durability of benefit
Nevertheless, Li-ESWT stands as one of the most promising innovations in contemporary ED therapy.
Vacuum and Negative Pressure Devices
While traditional vacuum erection devices continue to serve as a reliable mechanical alternative, newer modifications aim to improve comfort, efficiency, and ease of use. These devices remain particularly beneficial for men with contraindications to pharmacotherapy or with post-surgical erectile dysfunction.
Their physiological effect—enhancing cavernosal oxygenation—may also provide protective anti-fibrotic benefits, making them potentially valuable as adjunctive therapy in early or preventive settings.
Penile Prostheses: The Gold Standard for Refractory ED
Despite advances in regeneration and energy-based therapies, penile implants remain unmatched for predictability and user satisfaction in men with severe, refractory ED. The latest generation of prostheses features enhanced durability, reduced infection rates, and more naturalistic functionality.
While prosthetic surgery is invasive and irreversible, the reliability and success rates remain exceptionally high, positioning it as an essential option for men who have exhausted conservative measures.
Pharmacologic Innovations: Beyond First-Generation PDE5 Inhibitors
Pharmacotherapy remains the backbone of ED management, but innovation in this domain continues to evolve, particularly in optimizing delivery methods, improving onset times, and minimizing systemic side effects.
Rapid-Onset and Alternative PDE5I Formulations
Novel formulations—such as oral dispersible films (ODFs), sublingual preparations, and fast-dissolving tablets—aim to optimize convenience and onset of action. These formulations are receiving increased attention due to:
- patient preference for discreet administration
- potential improvements in bioavailability
- more predictable absorption profiles
While these agents do not fundamentally change the mechanism of ED treatment, they improve usability and patient adherence, which in clinical practice can be nearly as important as pharmacologic potency.
Hormonal Therapies in Select Populations
Recognizing that hypogonadism contributes to ED in a subset of men, testosterone replacement therapy (TRT) remains a cornerstone in managing androgen-deficient individuals. Innovations in transdermal, buccal, and injectable formulations seek to achieve stable physiological levels with minimal fluctuations.
Researchers are also investigating selective androgen receptor modulators (SARMs) as targeted therapies with potentially fewer side effects. Though still experimental, SARMs may eventually offer a more refined hormonal approach to ED in hypogonadal men.
Novel Molecular Targets
Future pharmacologic classes aim to address limitations inherent to PDE5 inhibitors. Experimental drugs include:
- soluble guanylyl cyclase stimulators
- rho-kinase inhibitors
- melanocortin receptor agonists
These agents explore pathways beyond nitric oxide signaling, creating potential solutions for patients with endothelial dysfunction or compromised nitric oxide synthesis.
Psychosexual and Behavioral Innovations: The Human Side of ED Therapy
ED is never exclusively physical; psychological and interpersonal factors play a substantial role. Innovations in this domain may not involve cutting-edge molecular biology, but they are no less important.
Integrative Therapeutic Models
Current research supports blended approaches combining medical treatment with cognitive-behavioral therapy (CBT) or couples therapy. This holistic model recognizes that restoring erectile function is only one component of healthy sexual relationships. Addressing anxiety, communication barriers, and partner dynamics enhances treatment outcomes and long-term satisfaction.
Digital Health and Telemedicine
Telemedicine has rapidly reshaped ED management, offering:
- access to sexual health specialists
- discreet consultations
- algorithm-driven diagnostic tools
While digital platforms cannot replace comprehensive clinical evaluation in all cases, they have democratized access to care and reduced stigma associated with discussing sexual dysfunction.
The Future Landscape: Toward Precision Sexual Medicine
The direction of ED therapy is unmistakably trending toward personalized, regenerative, and multimodal care. Advances in genomics, molecular profiling, and imaging technologies will likely refine diagnostic accuracy and allow treatments to be tailored to individual physiological and molecular profiles.
This shift promises not only more effective therapy but a more nuanced understanding of what ED truly represents: a multifactorial condition that mirrors broader systemic health.
Key future directions include:
- multimodal treatment combining biologics + devices + pharmacotherapy
- precision regenerative therapy customized to patient-specific deficits
- enhanced imaging of penile microvasculature for early detection of dysfunction
Ultimately, ED treatment is moving away from “fixing erections” and toward restoring comprehensive sexual health—a broader, more humanistic goal aligned with contemporary patient expectations.
Conclusion
Erectile dysfunction treatment is undergoing a profound transformation. The long-standing reliance on pharmacotherapy is giving way to a more diverse, mechanistic, and regenerative approach. Emerging therapies such as stem cell injections, PRP, gene therapy, and shockwave treatments offer hope for men unresponsive to traditional drugs. Meanwhile, innovations in pharmacology, devices, and psychosexual care provide a richer toolkit for clinicians seeking to personalize therapy.
This evolution reflects a deeper truth: ED is not merely an isolated condition but a systemic manifestation of vascular, metabolic, and neurogenic health. As research continues to unravel these connections, treatment will increasingly focus on disease modification rather than symptom management.
Modern sexual medicine is shifting decisively toward efficacy, durability, and holistic well-being—and the innovations explored in this review suggest that the future of ED therapy may be not just functional but truly restorative.
FAQ
1. Are regenerative therapies like stem cells or PRP proven treatments for erectile dysfunction?
They show promising early results, but most regenerative therapies are still considered investigational. Controlled trials indicate safety and potential benefits, but long-term data and standardization are necessary before they become mainstream.
2. Can energy-based treatments such as shockwave therapy replace PDE5 inhibitors?
Not yet. Shockwave therapy can improve erectile function, especially in men who respond poorly to PDE5 inhibitors, but it is generally considered an adjunct or alternative—not a replacement.
3. Is gene therapy a realistic future option for ED, or just experimental science?
Gene therapy is still experimental but increasingly feasible. Early trials show that targeted gene modulation can improve erectile function, but widespread clinical adoption will require extensive safety validation and regulatory approval.