Introduction
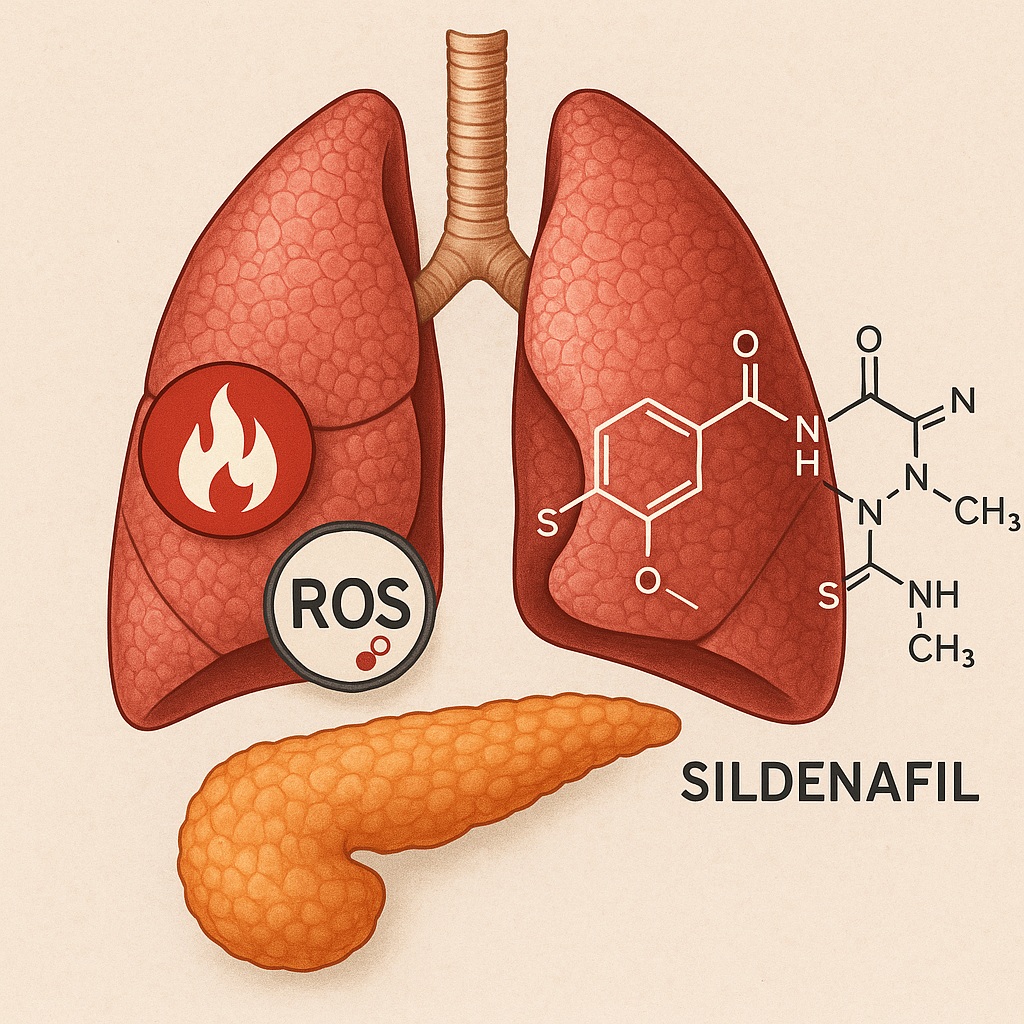
Medicine has an odd sense of irony. The same molecule that made headlines for restoring erectile function in aging men now appears to calm a very different kind of overreaction—an inflamed, gasping lung. Sildenafil, the well-known phosphodiesterase type 5 (PDE5) inhibitor, has long been associated with vascular relaxation and pulmonary hypertension therapy. Yet, recent studies have begun to uncover its less glamorous, but potentially lifesaving, capacity to dampen inflammation and oxidative injury in the context of systemic diseases.
Among the most catastrophic of these conditions is severe acute pancreatitis (SAP)—a sudden, devastating inflammatory process that originates in the pancreas but often spreads like wildfire to remote organs. Of these secondary targets, the lungs are particularly vulnerable, and acute lung injury (ALI) remains a leading cause of mortality in SAP.
The study “Effects of sildenafil on inflammatory injury of the lung in sodium taurocholate-induced severe acute pancreatitis rats” provides a meticulous exploration of this phenomenon. Using a well-established rat model, the researchers evaluated whether sildenafil could mitigate SAP-induced pulmonary inflammation and oxidative stress. The findings, while confined to animal data, shed light on an intriguing new therapeutic direction—repurposing sildenafil as an anti-inflammatory and endothelial-protective agent.
This article unpacks the pathophysiology behind the model, the experimental insights, and the potential clinical implications of this molecular crossover between vasodilation and immunomodulation.
The Systemic Storm: Understanding Severe Acute Pancreatitis and Its Pulmonary Fallout
Severe acute pancreatitis represents the cruel side of inflammation—a runaway process where the pancreas essentially digests itself. The initial injury begins when digestive enzymes become prematurely activated within pancreatic acinar cells, leading to autodigestion, cell death, and the release of pro-inflammatory mediators.
This localized chaos quickly spirals into a systemic inflammatory response syndrome (SIRS). Cytokines such as tumor necrosis factor-alpha (TNF-α), interleukin-1β (IL-1β), and interleukin-6 (IL-6) flood the circulation, transforming a pancreatic injury into a full-body crisis.
The lungs, with their vast endothelial surface and delicate alveolar-capillary network, are particularly susceptible to this cytokine storm. The result is increased vascular permeability, pulmonary edema, and infiltration of neutrophils—hallmarks of acute lung injury (ALI) and, in its severe form, acute respiratory distress syndrome (ARDS).
Pathophysiologically, SAP-induced lung injury involves:
- Microcirculatory dysfunction, leading to hypoxia and endothelial damage.
- Oxidative stress, mediated by excessive reactive oxygen species (ROS) production.
- Neutrophil activation, amplifying tissue injury through proteolytic enzymes and cytokine release.
This vicious cycle ultimately disrupts gas exchange, leading to respiratory failure. Unfortunately, supportive care remains the mainstay of therapy—oxygen, fluids, and mechanical ventilation—while specific pharmacologic strategies to curb the inflammatory cascade have remained elusive.
It is within this therapeutic void that sildenafil, an unlikely contender, enters the stage.
Sildenafil: From Vasodilator to Immunomodulator
Sildenafil’s pharmacological fame rests on its inhibition of PDE5, the enzyme responsible for degrading cyclic guanosine monophosphate (cGMP). By preventing cGMP breakdown, sildenafil enhances nitric oxide (NO)-mediated vasodilation, improving perfusion and reducing pulmonary artery pressure. This mechanism underlies its established roles in erectile dysfunction and pulmonary hypertension.
However, emerging research has revealed that sildenafil’s effects extend well beyond smooth muscle relaxation. Elevated cGMP levels exert anti-inflammatory, anti-apoptotic, and antioxidative effects through several molecular pathways. These include:
- Inhibition of NF-κB activation, a central transcription factor governing cytokine expression.
- Reduction of neutrophil adhesion and infiltration, preserving endothelial integrity.
- Enhancement of antioxidant enzyme activity, such as superoxide dismutase (SOD) and catalase.
In the context of SAP-induced ALI, where endothelial dysfunction and oxidative damage dominate, these mechanisms position sildenafil as a potentially powerful modulator of inflammatory injury.
The Experiment: Modeling Pancreatitis and Measuring Lung Protection
In the referenced study, researchers employed the sodium taurocholate (NaT)-induced pancreatitis model, one of the most reproducible and clinically relevant methods for mimicking severe acute pancreatitis in rats. Sodium taurocholate, a bile salt, is retrogradely injected into the pancreatic duct, triggering enzymatic activation, acinar necrosis, and systemic inflammation.
The experimental groups included:
- A control group (sham-operated rats).
- A SAP group, receiving sodium taurocholate to induce pancreatitis.
- A sildenafil-treated SAP group, receiving sildenafil after SAP induction.
The team evaluated a range of biochemical and histological markers to assess both pancreatic and pulmonary injury, including:
- Serum amylase and lipase (pancreatic injury markers).
- Pro-inflammatory cytokines: TNF-α, IL-1β, and IL-6.
- Oxidative stress markers: malondialdehyde (MDA) levels and antioxidant enzyme activity (SOD, glutathione peroxidase).
- Histopathological scoring for edema, leukocyte infiltration, and alveolar damage.
The lungs, as anticipated, bore the brunt of systemic inflammation in the SAP group, showing alveolar septal thickening, neutrophil infiltration, and hemorrhage. But in sildenafil-treated rats, these injuries were markedly attenuated.
Mechanisms of Protection: The Multifaceted Role of Sildenafil
1. Modulating Inflammation
Sildenafil’s primary benefit in this model was its ability to suppress pro-inflammatory cytokine production. Levels of TNF-α, IL-1β, and IL-6 were significantly lower in treated rats compared with untreated SAP counterparts. These cytokines are known amplifiers of neutrophil recruitment and endothelial injury; thus, their reduction suggests a damping of the systemic inflammatory response.
Moreover, sildenafil appeared to interfere with NF-κB signaling, a master switch in inflammation. By maintaining cGMP-mediated inhibition of NF-κB activation, sildenafil likely curbed the transcription of downstream inflammatory genes, blunting the cytokine cascade at its source.
2. Reducing Oxidative Stress
Oxidative damage, driven by excessive ROS, is a central feature of SAP-induced lung injury. In the study, untreated SAP rats exhibited a sharp rise in malondialdehyde—a marker of lipid peroxidation—and a decline in endogenous antioxidants such as SOD and glutathione peroxidase. Sildenafil treatment reversed these trends, suggesting a restoration of the oxidative balance.
The mechanism likely involves the NO–cGMP pathway’s ability to scavenge free radicals and enhance mitochondrial stability, reducing cellular stress.
3. Protecting Endothelial and Alveolar Integrity
Endothelial cells serve as the gatekeepers of vascular permeability. In SAP, cytokine and ROS-mediated damage disrupts endothelial tight junctions, leading to pulmonary edema. Sildenafil preserved these structures, as evidenced by reduced lung wet/dry ratios and improved histological architecture.
This preservation may result from enhanced endothelial nitric oxide synthase (eNOS) activity, which maintains vascular tone and barrier function. Thus, sildenafil acts not only as a vasodilator but as an endothelial stabilizer, preventing the vascular leak central to ALI.
The Broader Implications: Rethinking an Old Drug
While this experiment was confined to rats, its implications extend to human critical care. Acute pancreatitis remains a condition of frustrating therapeutic limitation—no specific pharmacologic intervention has proven consistently effective in reducing mortality. Supportive management remains the rule, even as the pathophysiology is well understood.
Sildenafil’s dual capacity to modulate vascular tone and suppress inflammation opens intriguing clinical possibilities. If similar effects were observed in humans, PDE5 inhibitors could theoretically:
- Mitigate acute respiratory distress syndrome (ARDS) secondary to pancreatitis or sepsis.
- Reduce microvascular thrombosis and improve tissue oxygenation.
- Protect other organs from secondary ischemic injury, such as the kidneys and liver.
Moreover, sildenafil’s established pharmacokinetic and safety profiles make it a prime candidate for drug repurposing—an increasingly valuable strategy in modern medicine, where time and cost constraints often limit the development of novel agents.
From Bench to Bedside: The Challenges of Translation
Despite the promise, several hurdles separate experimental success from clinical application. Animal models, while invaluable, rarely capture the full complexity of human disease. The sodium taurocholate model induces an abrupt and uniform injury, whereas human SAP often evolves over days, influenced by genetics, comorbidities, and variable systemic responses.
Additionally, the timing and dosage of sildenafil administration require careful optimization. Administered too late, after endothelial and parenchymal destruction have set in, its effects may be minimal. Administered too early, it could potentially exacerbate hypotension—a dangerous outcome in critically ill patients.
Another consideration is the multifaceted pharmacology of sildenafil. By enhancing nitric oxide signaling, the drug could, in theory, worsen capillary leak if applied indiscriminately. Thus, translating these findings will require precise dosing strategies and, ideally, targeted delivery systems to the pulmonary microcirculation.
Finally, clinical trials in this domain face ethical and logistical challenges. SAP is unpredictable, its progression rapid. Enrolling and monitoring critically ill patients under standardized protocols is notoriously difficult. Yet, without such trials, the translational bridge remains incomplete.
Sildenafil Beyond the Pancreas: A Broader Anti-Inflammatory Role
The findings from this study align with a growing body of evidence that PDE5 inhibition exerts broad-spectrum anti-inflammatory effects across various organs. Experimental models have shown sildenafil reducing:
- Renal ischemia-reperfusion injury, by improving microvascular perfusion and reducing oxidative stress.
- Myocardial infarct size, through preconditioning-like effects on mitochondria.
- Cerebral edema, by stabilizing the blood-brain barrier.
In essence, sildenafil’s mechanism appears to converge on the preservation of microvascular integrity and mitochondrial function, two common denominators in many inflammatory and ischemic conditions.
If future research continues to validate these pleiotropic effects, sildenafil may graduate from a niche cardiovascular and urological drug to a systemic anti-inflammatory adjunct—a pharmacologic multitool in the critical care physician’s arsenal.
Clinical Perspective: The Case for Repurposing Sildenafil
Drug repurposing is one of the most pragmatic and cost-effective paths to innovation in medicine. Sildenafil exemplifies this paradigm shift: an old drug with a new life. The advantages are obvious—its safety is well documented, its pharmacodynamics understood, and its manufacturing already optimized.
In the context of critical care, where new drug development often lags behind clinical need, sildenafil’s repositioning as an anti-inflammatory and organ-protective agent could be revolutionary.
However, this requires cautious optimism. Before sildenafil can be endorsed for SAP-associated ALI or similar inflammatory syndromes, rigorous human trials must establish:
- Optimal dosing strategies to balance vasodilatory and anti-inflammatory effects.
- Safety profiles in hemodynamically unstable patients.
- Efficacy endpoints, including mortality reduction, ventilator-free days, and inflammatory marker trends.
In short, the molecule has promise, but medicine—rightly—demands proof.
Conclusion
Sildenafil’s journey from treating erectile dysfunction to potentially mitigating life-threatening inflammatory lung injury reflects the evolution of pharmacology itself—from targeting isolated symptoms to addressing systemic dysfunctions.
The study on sodium taurocholate-induced SAP in rats offers compelling evidence that sildenafil can alleviate pulmonary inflammation, reduce oxidative stress, and preserve endothelial integrity in one of the most devastating models of systemic inflammation. While translation to human therapy remains an aspiration rather than a reality, the mechanistic logic is sound and the biological plausibility strong.
Perhaps, in the near future, sildenafil’s role in critical care will no longer raise eyebrows but expectations. After all, in medicine, as in life, it’s not where you start that matters—but how many systems you can protect along the way.
FAQ: Sildenafil and Lung Injury in Severe Acute Pancreatitis
1. How does sildenafil protect the lungs during severe acute pancreatitis?
Sildenafil increases intracellular cGMP by inhibiting PDE5, leading to vasodilation and anti-inflammatory effects. It suppresses pro-inflammatory cytokines (TNF-α, IL-1β, IL-6), reduces oxidative stress, and preserves endothelial and alveolar integrity—thereby mitigating acute lung injury.
2. Is sildenafil currently used in clinical practice for pancreatitis-related lung injury?
No. Its use in this context remains experimental. The evidence so far comes from animal models, though the results are promising enough to justify future clinical trials in humans.
3. Could sildenafil be harmful in severe inflammatory states?
Potentially, if used inappropriately. Its vasodilatory properties could lower blood pressure or exacerbate fluid leakage in unstable patients. Therefore, careful dosing and patient selection would be critical in any future clinical application.