Introduction
Erectile dysfunction (ED) is one of the most common conditions encountered in men’s health, affecting up to half of men over the age of 40 to varying degrees. While the condition is often simplistically attributed to aging or psychological stress, the underlying physiology is far more complex. Vascular disease, endocrine imbalance, neurological injury, and even systemic inflammation all converge on the erectile process, which requires seamless coordination between hormonal signaling, endothelial function, smooth muscle tone, and neural input.
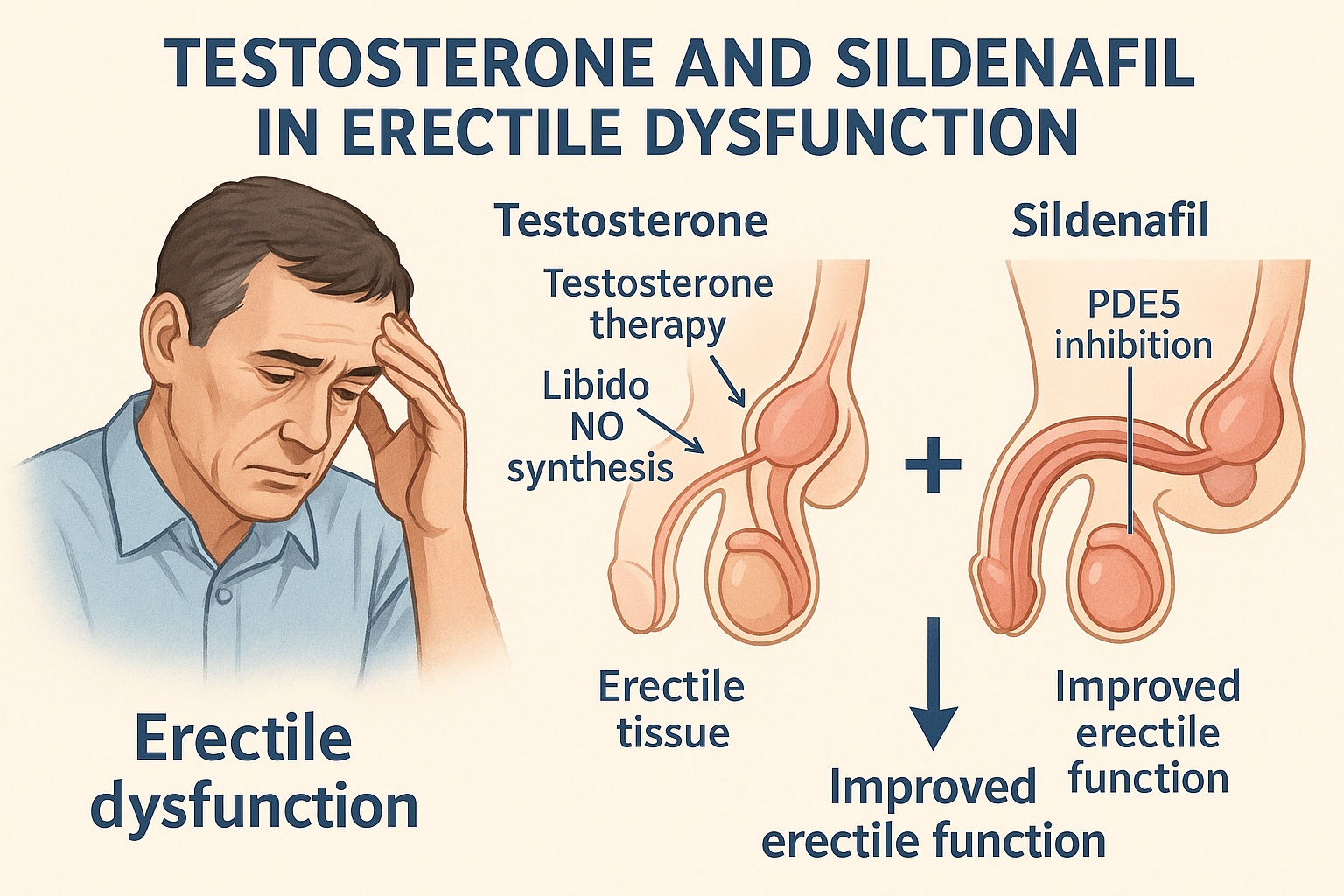
Among the most important contributors is testosterone deficiency (TD), also termed male hypogonadism. Testosterone is essential not only for libido but also for the structural and functional integrity of erectile tissue. Men with low testosterone frequently present with fatigue, reduced sexual desire, and variable erectile responses. Importantly, they also respond poorly to phosphodiesterase type 5 inhibitors (PDE-5 inhibitors) such as sildenafil, tadalafil, or vardenafil — drugs that otherwise revolutionized ED treatment.
This paradox raises a critical question: should testosterone replacement therapy (TRT, or TST for supplementation therapy) be combined with sildenafil in men with testosterone deficiency? A published case report examined precisely this issue, documenting the long-term management of a man with ED and TD treated with both testosterone and sildenafil. The findings highlight the limitations of single-agent therapy and illustrate how combined pharmacology can achieve durable improvement.
This article will explore the scientific rationale, clinical evidence, and practical lessons of this approach. By the end, the reader will understand why testosterone and sildenafil, though distinct in action, can complement each other in restoring erectile function — and why neither should be overestimated as a panacea.
Testosterone Deficiency and Erectile Function
Testosterone exerts profound effects on sexual physiology. In the central nervous system, it enhances libido, sexual motivation, and nocturnal penile tumescence. At the peripheral level, it regulates endothelial nitric oxide synthase (eNOS), modulates smooth muscle responsiveness, and maintains the structure of the corpus cavernosum. Chronic deficiency leads to fibrosis, impaired relaxation, and diminished penile blood inflow.
The causes of testosterone deficiency are numerous. Primary testicular failure, pituitary dysfunction, chronic illness, obesity, metabolic syndrome, and aging itself can all reduce circulating testosterone. Symptoms extend beyond sexual function: fatigue, mood changes, decreased muscle mass, and osteoporosis reflect the systemic nature of hypogonadism.
When testosterone levels are low, PDE-5 inhibitors often fail. This is because sildenafil and its class rely on nitric oxide–mediated production of cyclic guanosine monophosphate (cGMP). If the upstream signal — namely testosterone’s permissive role in NO synthesis and signaling — is absent, sildenafil has little to amplify. Clinical frustration often ensues: men are prescribed sildenafil, experience minimal improvement, and remain dissatisfied. This therapeutic gap has fueled interest in combination therapy.
Mechanisms of PDE-5 Inhibition
Sildenafil’s success lies in its elegant pharmacology. By inhibiting PDE-5, it prevents degradation of cGMP in smooth muscle cells of the corpus cavernosum. Elevated cGMP maintains smooth muscle relaxation, permitting arterial inflow and venous occlusion — the hemodynamic hallmarks of erection.
However, this cascade requires adequate NO release from nerve endings and endothelium. Without sufficient NO, little cGMP is generated, leaving PDE-5 inhibition ineffective. Testosterone deficiency disrupts NO synthase expression and reduces responsiveness of cavernosal tissue. Thus, sildenafil cannot rescue erectile capacity if the hormonal substrate is missing.
In contrast, when testosterone levels are normalized, the NO-cGMP pathway is restored, and sildenafil regains its potency. This mechanistic synergy explains why combination therapy has become a subject of considerable clinical interest.
Case Study: Long-Term Combination Therapy
The reported case involved a man with persistent ED despite sildenafil therapy. Laboratory evaluation revealed testosterone deficiency, confirming that hormonal imbalance was contributing to his condition. Testosterone supplementation was initiated, and sildenafil was continued.
Over time, the patient demonstrated remarkable improvement in erectile quality, sexual satisfaction, and overall well-being. Importantly, these benefits were sustained during long-term follow-up, suggesting that combination therapy provided durable restoration of function rather than transient relief.
This case illustrates several key principles:
- Testosterone replacement alone may restore libido but not erections if vascular responsiveness remains impaired.
- Sildenafil alone may improve hemodynamics but fails if upstream signaling is deficient.
- Together, they address both sides of the erectile equation: hormonal drive and vascular mechanics.
The therapeutic lesson is clear: in men with ED and documented hypogonadism, failure of PDE-5 inhibitors should prompt consideration of testosterone evaluation and supplementation.
Broader Evidence: Beyond a Single Case
While case reports provide anecdotal insights, broader clinical studies reinforce the concept of synergy. Randomized controlled trials have shown that TRT improves response rates to PDE-5 inhibitors in hypogonadal men. Patients who previously failed sildenafil often achieve satisfactory erections after testosterone is normalized.
Meta-analyses confirm this pattern, reporting improved International Index of Erectile Function (IIEF) scores in men receiving combination therapy compared to PDE-5 inhibitors alone. The benefits are most pronounced in men with baseline testosterone below physiological range, reinforcing the importance of patient selection.
That said, testosterone supplementation is not universally benign. Concerns about erythrocytosis, prostate effects, and cardiovascular risk continue to spark debate. Thus, while combination therapy can be highly effective, it must be pursued judiciously, with careful monitoring and individualized assessment.
The Physiology of Synergy
Understanding why sildenafil and testosterone work better together requires revisiting basic physiology. Testosterone promotes NO synthase activity, enhances penile smooth muscle content, and reduces deposition of collagen that otherwise stiffens erectile tissue. In parallel, sildenafil ensures that the NO produced is not wasted, amplifying the signal downstream.
This dual mechanism — restoration of upstream signaling and preservation of downstream effect — creates a functional synergy greater than either drug alone. It is, in essence, a pharmacological duet where testosterone sets the melody and sildenafil provides the rhythm.
This is not merely poetic. The clinical implications are profound: men once consigned to frustration and failed therapies can experience renewed function, provided both aspects of their pathophysiology are addressed.
Risks and Limitations
No discussion of combination therapy would be complete without an examination of risks. Testosterone supplementation can elevate hematocrit, potentially increasing thrombotic risk. It can stimulate prostate tissue, raising concerns about benign prostatic hyperplasia progression or prostate cancer. Fluid retention, acne, and sleep apnea exacerbation are additional considerations.
Sildenafil, for its part, is generally safe but not without drawbacks. Headache, flushing, nasal congestion, and dyspepsia are common. Rarely, visual disturbances or hearing loss occur. Importantly, sildenafil is contraindicated in men using nitrates, as the combination can cause life-threatening hypotension.
Together, the two therapies require vigilance. Baseline and periodic monitoring of testosterone, hematocrit, prostate-specific antigen (PSA), and cardiovascular status is essential. The goal is to harness benefit while minimizing risk — a balance achievable through disciplined clinical practice.
Clinical Practice Implications
From a practical standpoint, several lessons emerge:
- Evaluate testosterone in ED non-responders: Men who fail PDE-5 inhibitors should undergo hormonal evaluation.
- Prioritize individualized therapy: Not all men with ED and low testosterone require combination treatment. Decisions should weigh symptom burden, comorbidities, and patient preferences.
- Monitor systematically: Combination therapy demands follow-up. Laboratory testing, prostate assessment, and cardiovascular screening are not optional.
- Manage expectations: Patients must understand that combination therapy improves function but is not a cure-all. Psychological, relational, and lifestyle factors still play roles in sexual health.
In short, sildenafil plus testosterone can transform outcomes, but only when embedded in a broader framework of patient-centered care.
A Note on Long-Term Outcomes
The long-term outlook of men receiving both therapies remains an active area of investigation. Case reports and small trials suggest sustained benefit, but larger longitudinal studies are needed. Of particular importance is clarifying whether TRT in combination with sildenafil alters cardiovascular or prostate cancer risk over decades.
Until such data are available, clinicians must rely on intermediate markers, shared decision-making, and prudent caution. The balance between quality of life and long-term safety remains delicate.
Conclusion
The story of sildenafil and testosterone in erectile dysfunction is a story of complementarity. Each drug alone can disappoint when the underlying physiology is imbalanced. Together, they restore both hormonal drive and vascular mechanics, achieving results unattainable in isolation.
The case study of long-term combination therapy underscores this point: in men with ED and hypogonadism, sildenafil becomes effective once testosterone is normalized, and testosterone achieves fuller impact when sildenafil sustains vascular responsiveness.
Yet caution is warranted. Risks exist, monitoring is essential, and not all patients are suitable candidates. The clinician’s task is to identify who stands to benefit, to tailor therapy carefully, and to ensure ongoing surveillance.
For men debilitated by ED and failed therapies, however, the message is one of hope. Combination treatment is not a miracle, but it is a potent partnership — one that reaffirms the importance of understanding physiology before prescribing pharmacology.
FAQ
1. Why do some men not respond to sildenafil alone?
Because sildenafil requires adequate nitric oxide production to work. In men with testosterone deficiency, NO synthesis is impaired, leaving sildenafil with little effect to amplify.
2. Does testosterone therapy cure erectile dysfunction?
Not entirely. While testosterone restores libido and supports penile tissue health, many men still require PDE-5 inhibitors for optimal erections. TRT addresses part of the problem, not the whole.
3. Is combination therapy safe for long-term use?
Combination therapy can be safe when carefully monitored, but risks exist. Men must undergo regular follow-up including testosterone levels, blood counts, prostate assessments, and cardiovascular evaluation. The therapy should always be individualized.