Introduction
Erectile dysfunction (ED) remains one of the most prevalent male sexual health concerns, affecting up to 50% of men over the age of 50. Defined as the persistent inability to attain or maintain an erection sufficient for satisfactory sexual performance, ED is more than an inconvenience: it is a sentinel marker of vascular, metabolic, and psychological health. The global prevalence of ED mirrors the rise of metabolic syndrome, obesity, diabetes, and cardiovascular disease, making its management both a personal and a public health priority.
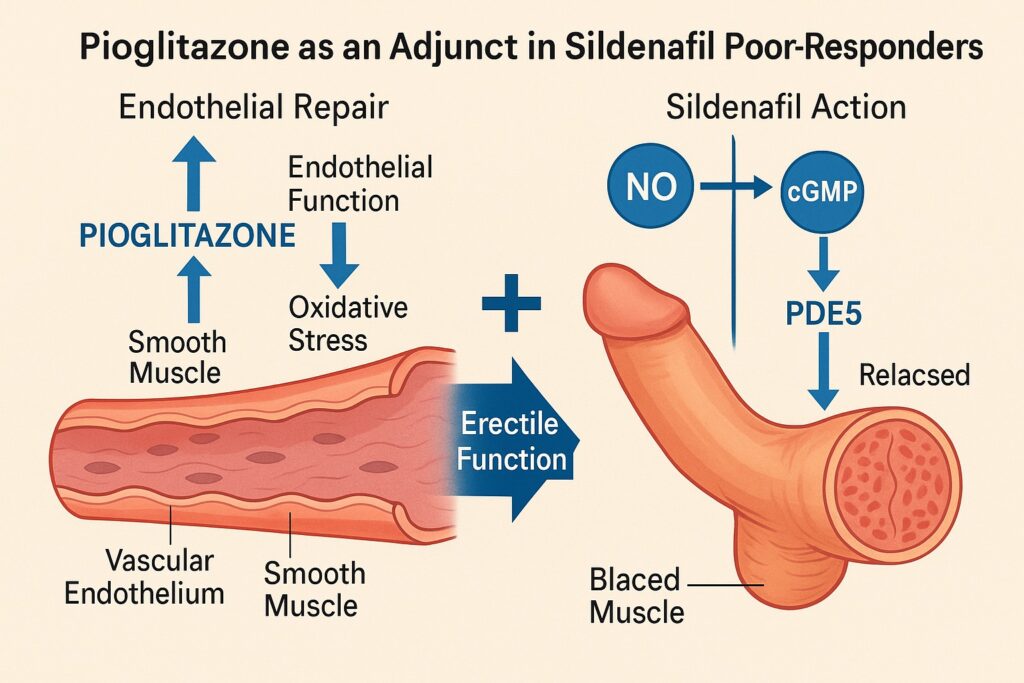
Since their introduction in the late 1990s, phosphodiesterase type 5 (PDE5) inhibitors—notably sildenafil—have revolutionized the treatment of ED. By enhancing nitric oxide–mediated cyclic guanosine monophosphate (cGMP) signaling in the corpus cavernosum, these agents restore penile vasodilation and rigidity in the majority of cases. However, the story is far from complete. Between 30% and 40% of patients fail to respond adequately to PDE5 inhibitors, particularly those with underlying diabetes mellitus, severe endothelial dysfunction, or advanced cardiovascular disease. These “poor-responders” represent one of the most challenging subsets in urology and andrology.
The 2008 randomized controlled study by Gholamine and colleagues explored an innovative approach: the addition of pioglitazone, a peroxisome proliferator-activated receptor gamma (PPAR-γ) agonist traditionally used in type 2 diabetes, as an adjunct to sildenafil in patients with ED who responded poorly to PDE5 inhibitors alone. Their findings not only expand therapeutic possibilities but also underscore the pathophysiological overlap between ED, insulin resistance, and vascular health. This article unpacks the rationale, results, and implications of this important study, with an eye toward clinical translation.
Pathophysiology of Erectile Dysfunction: More Than a Penile Problem
To appreciate why pioglitazone might have a role in ED, one must first revisit the biology of erection. Penile erection is a hemodynamic event governed by neurovascular and endothelial integrity. Parasympathetic stimulation triggers nitric oxide release, activating guanylate cyclase and increasing cGMP within smooth muscle cells. This cascade relaxes the trabecular smooth muscle and dilates penile arterioles, allowing cavernosal sinusoids to fill with blood. Venous outflow is compressed, sustaining rigidity.
In ED, this finely tuned system falters. Diabetes, hypertension, and hyperlipidemia promote endothelial dysfunction, reducing nitric oxide bioavailability. Oxidative stress impairs cGMP signaling, while atherosclerosis narrows cavernosal arteries. Neuropathy diminishes parasympathetic input. The result is a vascular bed that cannot adequately relax, regardless of central stimulation.
It is no surprise, then, that ED shares risk factors with cardiovascular disease. Indeed, ED often precedes coronary artery disease by years, acting as an early vascular barometer. In this context, simply boosting cGMP with PDE5 inhibitors may be insufficient when the endothelial machinery itself is broken. This is precisely where agents like pioglitazone enter the picture, targeting the vascular substrate of the problem rather than just amplifying its residual function.
The Rationale for Pioglitazone
Pioglitazone belongs to the thiazolidinedione (TZD) class, widely known for their role in improving insulin sensitivity in type 2 diabetes. By activating PPAR-γ, pioglitazone enhances glucose uptake in adipose tissue and muscle, reduces circulating free fatty acids, and improves lipid profiles. Yet beyond glycemic control, TZDs exert profound vascular effects.
PPAR-γ activation reduces vascular inflammation, enhances endothelial nitric oxide synthase (eNOS) activity, and diminishes oxidative stress. Animal studies have shown improved endothelial function and attenuated atherosclerosis with TZD therapy. In other words, pioglitazone acts at the very root of ED pathophysiology: restoring vascular health.
The hypothesis tested in the 2008 study was elegant: in sildenafil poor-responders, the problem may not be insufficient PDE5 inhibition but inadequate nitric oxide bioavailability and endothelial dysfunction. By repairing the vascular substrate with pioglitazone, sildenafil’s effect could be “unlocked,” improving erectile outcomes in otherwise refractory men.
Study Design and Methodology
The study was a prospective, randomized, controlled trial involving men with established ED who had shown poor response to sildenafil monotherapy. Patients were carefully screened to exclude confounding conditions such as severe neurological disorders, hypogonadism, or advanced psychiatric illness. Importantly, most participants had features of metabolic syndrome or diabetes, consistent with the pathophysiological rationale.
Participants were randomized into two groups:
- Control group: Continued sildenafil therapy.
- Intervention group: Received sildenafil plus pioglitazone.
Outcomes were assessed using the International Index of Erectile Function (IIEF), a validated multidimensional questionnaire, alongside patient self-reports of erection rigidity, frequency of successful intercourse, and satisfaction. Follow-up lasted several months, allowing for assessment of both efficacy and tolerability.
The use of standardized tools such as the IIEF ensured that results were not merely subjective impressions but quantifiable changes in erectile domains. Statistical analysis compared baseline and post-treatment scores within and between groups, providing robust evidence of efficacy.
Results: Pioglitazone Unlocks Sildenafil’s Potential
The results were compelling. Patients in the sildenafil + pioglitazone group demonstrated significant improvements in IIEF scores compared to the sildenafil-only group. Erectile rigidity, frequency of penetration, and successful intercourse attempts increased substantially. Satisfaction scores also improved, suggesting that benefits extended beyond function to the lived experience of intimacy.
Biochemically, improvements were consistent with enhanced endothelial function. Though the study was not designed as a mechanistic trial, ancillary measures suggested better glycemic control and improved lipid profiles in the pioglitazone group, lending credence to the hypothesis that vascular health underpinned the erectile gains.
Tolerability was acceptable. Pioglitazone’s known side effects—fluid retention, weight gain, and risk of heart failure in predisposed patients—were monitored but did not lead to significant discontinuations. The balance between risk and benefit appeared favorable, particularly in men with both ED and metabolic syndrome.
Mechanistic Insights: Why It Works
The synergy between pioglitazone and sildenafil highlights the multi-layered nature of erectile physiology. Sildenafil requires intact nitric oxide release to be effective, as it prevents cGMP breakdown but does not generate the signal itself. In endothelial dysfunction, nitric oxide production is impaired, limiting the drug’s substrate. Pioglitazone restores endothelial nitric oxide synthase activity, increases nitric oxide availability, and reduces oxidative stress that would otherwise degrade it.
In addition, pioglitazone may improve cavernosal blood flow by enhancing insulin sensitivity, reducing hyperglycemia-induced vascular damage, and mitigating chronic inflammation. The result is a penile vasculature that is more responsive to sildenafil, effectively converting poor-responders into responders.
This mechanistic model exemplifies the principle that complex disorders rarely yield to single-target interventions. Combination strategies—addressing both the symptom (erectile failure) and the root cause (endothelial dysfunction)—are more likely to succeed.
Clinical Implications
The clinical implications of this study are substantial. For urologists, andrologists, and primary care physicians managing ED, the findings provide a new therapeutic pathway for the notoriously challenging subset of PDE5 poor-responders. Instead of escalating sildenafil doses or turning prematurely to invasive options such as injection therapy or prosthesis implantation, clinicians may consider vascular-modulating adjuncts.
Patients with metabolic syndrome or diabetes stand to gain the most. These populations not only represent a large proportion of ED sufferers but also overlap with those at highest cardiovascular risk. By prescribing pioglitazone, physicians may improve both erectile function and cardiometabolic health, delivering dual benefit.
However, caution is necessary. Pioglitazone is not free from controversy. Concerns about fluid retention, bone fractures, and possible bladder cancer risk must be balanced against its benefits. Thus, careful patient selection is paramount: the ideal candidate is the middle-aged man with ED, insulin resistance, and no history of heart failure or bladder pathology.
Integration Into Broader ED Management
Pioglitazone should not be seen as a magic bullet but as part of a holistic ED management framework. Lifestyle modification—weight loss, exercise, smoking cessation, and diet—remains foundational. These interventions improve both vascular and sexual health, often rivaling pharmacological efficacy.
Other adjuncts may complement pioglitazone. Statins, angiotensin-converting enzyme inhibitors, and other vascular drugs have shown modest benefits in ED by improving endothelial function. The principle is the same: treat the penis as part of the vascular tree, not as an isolated organ.
Psychological support is equally important. Depression, anxiety, and relationship stress frequently accompany ED, and no amount of pharmacology can substitute for open communication, counseling, and partner involvement. Pioglitazone may improve vascular function, but intimacy requires a broader therapeutic lens.
Limitations and Future Research
The 2008 study, while pioneering, was not without limitations. Sample size was modest, follow-up relatively short, and mechanistic endpoints limited. Larger, multicenter trials are needed to confirm efficacy, explore long-term safety, and define optimal patient populations.
Further research should also address whether other PPAR-γ agonists share the same benefits, and whether combination strategies with newer antidiabetic agents (e.g., SGLT2 inhibitors or GLP-1 receptor agonists) might yield even greater improvements. The intersection of sexual medicine and metabolic pharmacology remains fertile ground for discovery.
Finally, female sexual dysfunction—a neglected cousin in this field—deserves attention. If pioglitazone improves endothelial function, might it also enhance arousal and lubrication in women with diabetes-related sexual dysfunction? Future studies should not ignore half the population.
Conclusion
Erectile dysfunction in sildenafil poor-responders represents one of the most frustrating clinical scenarios in sexual medicine. The 2008 randomized study of pioglitazone as an adjunct to sildenafil provides both hope and direction. By targeting endothelial dysfunction, pioglitazone restores the physiological foundation upon which PDE5 inhibitors act, converting failure into success for many patients.
The lesson is broader than one drug combination. It is a reminder that ED is not merely a penile problem but a vascular disorder reflecting systemic health. Treating the root cause, not just the symptom, yields the greatest rewards. As metabolic disease continues its global rise, integrative strategies like this one will be essential to restoring not only erectile function but also dignity, intimacy, and quality of life for millions of men worldwide.
FAQ
1. Why do some men not respond to sildenafil?
Poor response often reflects underlying endothelial dysfunction, diabetes, or vascular disease. Sildenafil enhances nitric oxide–cGMP signaling but cannot work effectively if nitric oxide production is impaired.
2. How does pioglitazone improve erectile function?
Pioglitazone improves endothelial health by enhancing nitric oxide availability, reducing oxidative stress, and improving insulin sensitivity. This restores the vascular substrate necessary for sildenafil to act.
3. Is pioglitazone safe for all men with ED?
No. While generally well tolerated, pioglitazone carries risks such as fluid retention, heart failure exacerbation, and possible bladder cancer. Careful patient selection is essential, and it should not replace foundational lifestyle and psychological interventions.


