Introduction
Erectile dysfunction (ED) remains one of the most frustrating disorders in andrology, not merely because it impairs sexual activity but also because it threatens male identity and self-confidence. The condition is defined as the persistent inability to achieve and maintain an erection sufficient for satisfactory sexual intercourse. Its prevalence increases with age, comorbidities such as diabetes and cardiovascular disease, and lifestyle factors. While oral phosphodiesterase type 5 (PDE5) inhibitors revolutionized treatment, not all men benefit. For a subset of patients, monotherapy—whether oral or injectable—offers little more than disappointment.
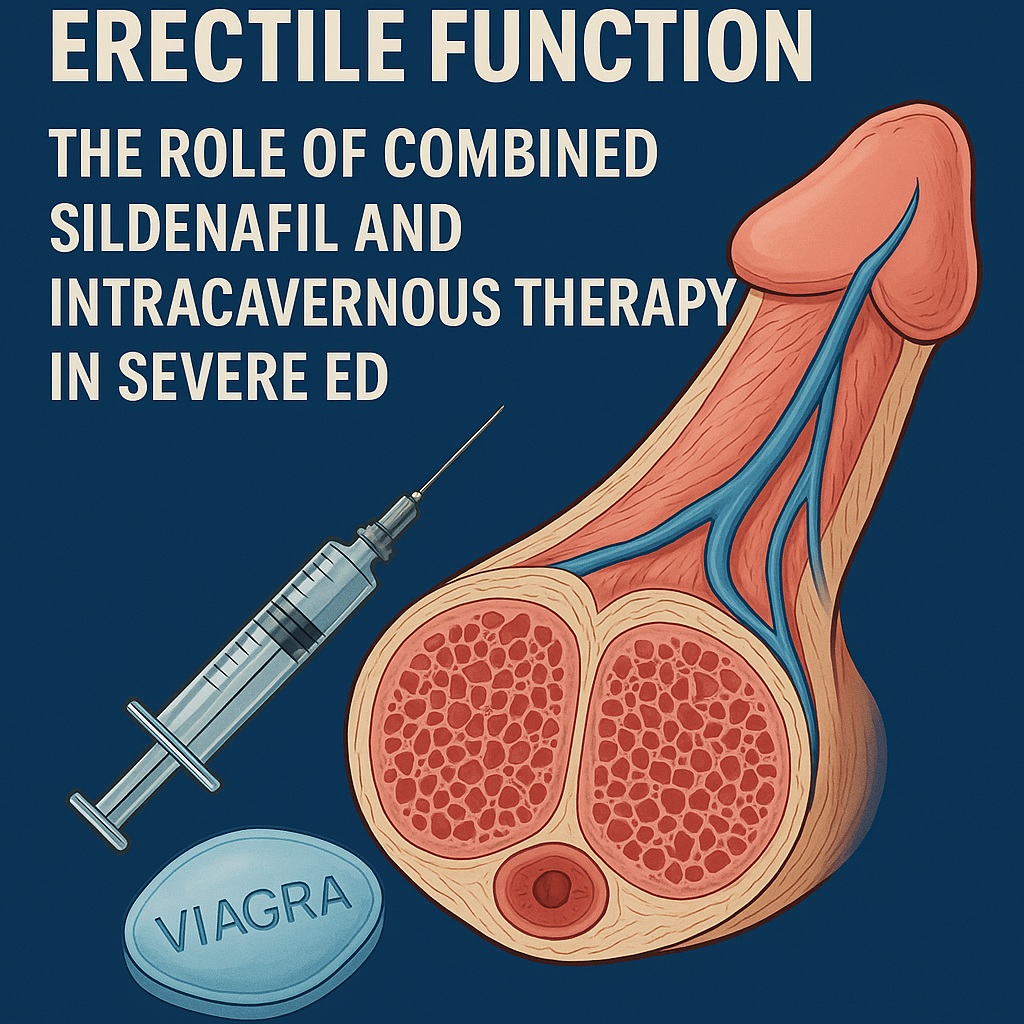
The study under review explored an alternative strategy: combining daily low-dose sildenafil with intracavernous injection (ICI) of a trimix solution containing papaverine, prostaglandin E1 (PGE1), and phentolamine. This approach moves away from episodic “on-demand” rescue therapy toward a chronic, synergistic regimen that aims to restore penile hemodynamics in otherwise refractory cases. The results raise important questions about redefining treatment goals and therapeutic perseverance in men with advanced ED.
Why Standard Therapies Fail
PDE5 inhibitors, such as sildenafil, enhance erections by sustaining cyclic GMP levels in penile smooth muscle, thereby facilitating nitric oxide–mediated vasodilation. They require intact neural and vascular pathways, as well as sexual stimulation, to be effective. Yet, in real practice, up to one-third of men fail to respond. Similarly, intracavernous injections of PGE1—which directly relax cavernosal smooth muscle through cAMP pathways—can also disappoint.
The common denominator of failure is often vascular pathology. Studies show that veno-occlusive dysfunction (VOD) and mixed arterial–veno-occlusive disease are particularly resistant to pharmacotherapy. When venous leak prevents adequate trapping of blood within the corpora cavernosa, even strong arterial inflow becomes futile. Such cases represent the therapeutic “hardcore,” where neither sildenafil nor PGE1 monotherapy provides reliable erections.
Beyond vascular disease, other barriers exist: psychological reluctance to inject the penis, comorbid diabetes, postsurgical changes after prostatectomy, and even cultural attitudes toward artificial erection. It is against this backdrop that combination therapy seeks to intervene—by striking at multiple biochemical pathways simultaneously.
The Rationale for Combination Therapy
Physiologically, erection requires orchestration of multiple signaling cascades. PDE5 inhibitors boost the nitric oxide–cGMP system, while papaverine inhibits multiple phosphodiesterases, increasing both cAMP and cGMP. PGE1 acts primarily through the cAMP pathway, and phentolamine blocks α-adrenergic tone, further promoting smooth muscle relaxation.
In theory, combining these agents should amplify the final common pathway: relaxation of cavernosal smooth muscle, increased arterial inflow, and efficient veno-occlusion. Practically, the idea is to administer lower doses of each drug, thereby minimizing side effects while maximizing synergistic efficacy.
Previous attempts at combination therapy often used on-demand regimens—sildenafil taken before intercourse plus ICI shortly thereafter. The study in question, however, tested a chronic protocol: daily sildenafil 25 mg and twice-weekly ICI with low-dose trimix for eight weeks. This approach shifts the paradigm from episodic intervention to continuous rehabilitation of penile hemodynamics.
Study Design: Patients and Methods
The trial enrolled 40 men with severe ED, average age about 51 years, all of whom had failed maximum-dose PDE5 inhibitors and ICI with PGE1 monotherapy. These were not casual non-responders but veterans of disappointment.
At baseline, erectile severity was measured using the Sexual Health Inventory for Men (SHIM-5). Penile vascular status was assessed with color Doppler ultrasonography (CDUS), recording peak systolic velocity (PSV), end-diastolic velocity (EDV), and resistance index (RI). Hemodynamic classifications were established as follows:
- Normal penile flow: PSV ≥ 30 cm/s, EDV ≤ 5 cm/s
- Arterial insufficiency: PSV < 30 cm/s, EDV normal
- Veno-occlusive dysfunction: PSV normal, EDV > 5 cm/s
- Mixed disease: abnormalities in both PSV and EDV
The treatment consisted of sildenafil citrate 25 mg daily plus ICI with 0.25 mL trimix twice weekly. Patients were instructed to attempt sexual activity at least twice per week, ensuring real-life applicability. After 8 weeks, outcomes were reassessed using the Erection Hardness Score (EHS), repeat CDUS, and the Erectile Dysfunction Inventory of Treatment Satisfaction (EDITS).
Results: Salvaging the Unresponsive
The baseline findings painted a grim picture. Of the 40 men, 65% had VOD, 13% had arterial insufficiency, 10% had mixed vascular disease, and only 13% had normal penile hemodynamics. In terms of erectile rigidity, many were incapable of reaching penetration hardness.
After eight weeks of combined therapy, 70% of patients (28/40) showed significant improvement. These men experienced:
- Higher SHIM-5 scores (from ~7.7 to ~21.8, p < 0.001)
- Shorter time to erection and longer erection duration
- Better penile blood flow with increased PSV and decreased EDV
- Higher EHS scores, with more patients achieving grade 3–4 rigidity
- Greater overall treatment satisfaction (EDITS index ~66%)
Non-responders were generally older, had longer histories of ED, and more often exhibited mixed vascular disease or severe VOD. In this subgroup, hemodynamic compromise proved too advanced for pharmacological salvage.
Adverse effects occurred in 43% of patients, most commonly penile pain, headache, and facial flushing. These side effects were tolerable and did not lead to widespread discontinuation, though they highlight the trade-off inherent in polypharmacy.
Discussion: Lessons Learned
The trial reinforces several critical lessons about ED management.
First, not all ED is created equal. While PDE5 inhibitors work wonders for many men, those with veno-occlusive pathology often need additional help. Expecting sildenafil alone to overcome profound venous leak is akin to patching a leaky dam with adhesive tape—it simply cannot hold.
Second, chronic combination therapy can rehabilitate penile hemodynamics. Rather than episodic pharmacological “shock therapy,” sustained low-dose treatment may remodel vascular responsiveness and improve tissue compliance. The idea resembles physiotherapy: consistent stimulation yields better long-term outcomes than sporadic effort.
Third, patient selection matters. Younger men with shorter ED duration and relatively preserved penile hemodynamics responded better. Older patients with long-standing VOD fared poorly. This underscores the importance of thorough vascular assessment before embarking on aggressive treatment.
Fourth, side effects are real but manageable. Polytherapy increases adverse events, but lower dosing strategies, as used here, may keep them tolerable. The key lies in balancing efficacy with safety, a perennial challenge in sexual medicine.
Finally, satisfaction is not only about rigidity. Some men rated the treatment unsatisfactory despite achieving firm erections, citing pain, unnatural feeling, or partner dissatisfaction. This highlights the psychological and relational dimensions of ED therapy, which cannot be ignored.
Clinical Implications
The findings suggest a pathway for men who have exhausted monotherapies. When PDE5 inhibitors or ICI with PGE1 fail, clinicians may consider:
- A structured trial of daily low-dose sildenafil to stabilize cGMP pathways.
- Adjunctive low-dose intracavernous trimix administered regularly to recruit multiple biochemical mechanisms.
- Careful monitoring of vascular status, side effects, and patient satisfaction.
However, this approach is not universally applicable. Men with profound veno-occlusive dysfunction, advanced age, or long-standing refractory ED may remain resistant. In such cases, surgical solutions such as penile prosthesis implantation may be the more realistic option.
Nonetheless, for the majority of men in the study, this combination regimen provided a second chance at sexual rehabilitation. It represents a bridge between pharmacological failure and surgical inevitability.
Conclusion
Severe ED unresponsive to on-demand monotherapy poses one of the most challenging dilemmas in sexual medicine. The study on combined chronic sildenafil and intracavernous trimix demonstrates that 70% of such men can be salvaged, with measurable improvements in penile hemodynamics, erection hardness, and patient satisfaction.
This strategy is not a panacea, and careful patient selection remains essential. Yet, it expands the therapeutic arsenal and underscores the principle that ED management must be multifaceted. Erection is not governed by a single molecule or drug class but by an orchestra of pathways. Sometimes, the only way to restore harmony is to combine instruments.
In the end, combination therapy offers a pragmatic message: when first-line options fail, persistence, creativity, and a willingness to blend pharmacological strategies can rescue function and, perhaps more importantly, restore hope.
FAQ
1. Why do some men not respond to Viagra or intracavernous PGE1?
Non-responders often have significant vascular abnormalities, particularly veno-occlusive dysfunction, where venous leak prevents adequate blood trapping in the penis. Without this mechanism, even strong vasodilation cannot sustain rigidity.
2. Is combined sildenafil and trimix therapy safe?
Yes, when used in carefully selected patients and under medical supervision. Adverse effects such as penile pain, headache, and flushing are common but usually tolerable. The regimen should always be individualized and closely monitored.
3. Does this therapy work for everyone with severe ED?
No. Younger men with shorter ED duration and less severe vascular compromise respond best. Those with advanced veno-occlusive disease or mixed pathology may remain refractory and may require surgical solutions such as penile prosthesis implantation.


