Introduction
Medicine advances in curious cycles. For decades, the prevailing paradigm has been “bench to bedside”—a straight highway where discoveries in basic science are transported into the clinical realm. Yet, as physicians and patients alike know, highways are prone to detours, delays, and even abrupt dead ends. A drug promising in mice often falters in humans. A biomarker dazzling in vitro may prove uninformative in real life. Enter reverse translational research (RTR), a framework that dares to invert the process: begin at the bedside, learn from real patients, and then return to the bench with questions that actually matter.
This model is not merely a semantic twist. It represents a necessary corrective to a drug discovery system struggling with spiraling costs, stagnating pipelines, and a disappointingly high failure rate in late-phase clinical trials. Reverse translation takes the chaos of clinical reality and channels it into sharper hypotheses, better models, and ultimately, therapies more attuned to the complexities of human biology.
In this article, we will navigate the conceptual foundations of RTR, examine its role in drug repurposing, explore its reliance on biomarkers and precision medicine, and acknowledge the challenges it must overcome. Finally, we will reflect on its potential to reshape the pharmaceutical landscape—a future where science listens more carefully to the patient before speaking for them.
The Problem with Traditional Translational Research
Traditional translational science emerged with noble intentions: shorten the distance between a laboratory breakthrough and a clinical application. Its “bench-to-bedside” mantra resonated with a generation of scientists, physicians, and funders who longed for speed and efficiency. And indeed, it has borne fruit. Cancer immunotherapy, statins, and mRNA vaccines all benefited from this highway.
Yet the cracks are undeniable. Translational research remains resource-intensive, slow, and plagued by attrition. More than 90% of molecules entering clinical testing never reach approval. The reasons are manifold:
- Preclinical models poorly mirror human physiology.
- Promising biomarkers in rodents often prove irrelevant in patients.
- Complex diseases, influenced by genetics, environment, and lifestyle, rarely conform to tidy laboratory constructs.
Moreover, the return on investment is underwhelming. Despite billions of dollars funneled into research and development, the rate of new drug approvals has not proportionally increased. Critics argue that translational research, for all its rhetoric, is failing to deliver at the scale needed.
Against this backdrop, reverse translational research steps in—not as a rejection of translational science, but as its evolution.
The Essence of Reverse Translational Research
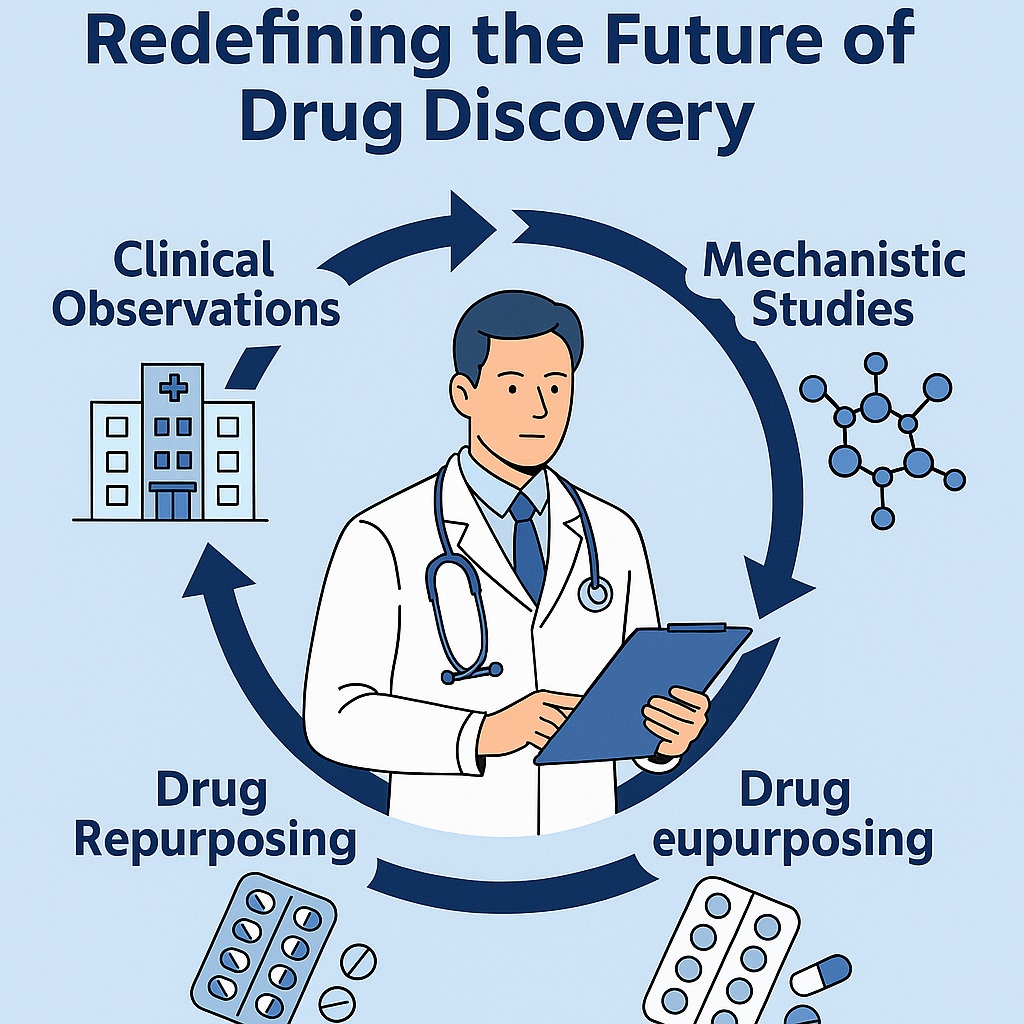
Reverse translation begins where traditional models end: with the patient. It collects observations from clinical practice—responses to therapies, unexpected side effects, variability in outcomes—and feeds these back into basic science. Instead of asking “what can this molecule do in humans?”, it asks “why did this human respond in this way, and what does it teach us about the underlying biology?”
The process is inherently cyclical. A patient’s unusual response to a drug generates a hypothesis, which inspires laboratory models, which in turn refine the therapy and lead back to improved clinical care. Each loop tightens the relationship between bedside reality and bench experimentation.
This approach has several advantages:
- Relevance: Hypotheses are rooted in genuine clinical phenomena.
- Efficiency: Research targets are informed by real-world outcomes, reducing wasted effort.
- Innovation: Unexpected findings, such as off-target drug effects, can inspire entirely new therapeutic avenues.
Perhaps most importantly, reverse translation reflects humility. It acknowledges that the human body is infinitely more complex than any model system and that true understanding often starts not with elegant theory but with messy reality.
The Need for Reverse Translational Research
One might ask: why invert the model now? The answer lies in the failures of preclinical science to predict clinical success. Numerous drugs shine in animal models only to collapse in human trials. Diseases such as Alzheimer’s, depression, and cancer have consumed vast resources with limited therapeutic payoff.
The limitations of animal models are central here. A mouse engineered to lack a gene may approximate one feature of a disease but will never embody the full human syndrome. Similarly, in vitro assays often strip away the complexity of cellular ecosystems, offering insights that are elegant but incomplete.
Reverse translational research offers a corrective lens. By focusing first on human responses, it ensures that subsequent laboratory investigations are tethered to clinical truth. For example, if 20% of patients respond exceptionally well to a drug while the rest do not, RTR can investigate why. Are there genetic variants? Specific biomarkers? Environmental exposures? Such insights can refine models, stratify patients, and accelerate precision medicine.
This is not to discard preclinical work, but to reposition it as a partner rather than dictator. The ultimate goal remains the same: effective, safe, and affordable therapies. RTR simply charts a more pragmatic course.
Drug Repurposing: A Natural Child of Reverse Translation
One of the most celebrated offspring of RTR is drug repurposing. The principle is straightforward: a medication designed for one condition proves useful in another. This is not accidental—it is the outcome of astute clinical observation followed by mechanistic exploration.
Sildenafil exemplifies this beautifully. Originally synthesized to treat angina, its vascular effects were underwhelming in that domain. However, clinicians noticed a rather striking side effect: improved erectile function. The observation returned to the laboratory, mechanisms were clarified, and sildenafil was reborn as Viagra—a blockbuster therapy for erectile dysfunction and later, pulmonary arterial hypertension.
This narrative repeats across medicine. Minoxidil, once an antihypertensive, found new fame as a hair growth agent. Thalidomide, notorious for its teratogenic effects, was reinvented as a therapy for multiple myeloma. Zidovudine, designed as an anticancer agent, became the first antiretroviral drug for HIV.
Drug repurposing exemplifies reverse translation at its best: clinical observation informs bench science, which in turn produces a refined and approved therapy. It saves time, reduces costs, and leverages existing safety data. In an era where pharmaceutical R&D is both exorbitant and inefficient, repurposing is not merely attractive—it is essential.
Biomarkers: The Compass of Reverse Translation
Biomarkers serve as the compass guiding RTR. They are measurable biological indicators—molecules, imaging signals, physiological parameters—that help decipher disease pathways, predict treatment responses, and monitor outcomes.
In reverse translational research, biomarkers bridge the gap between bedside observation and bench investigation. A patient who responds exceptionally well to a therapy may harbor a biomarker signaling heightened sensitivity. Conversely, an adverse reaction may reveal a biomarker of vulnerability. Identifying these clues allows researchers to design targeted experiments, validate mechanisms, and refine therapeutic strategies.
Examples abound. Cardiac troponins revolutionized the diagnosis of myocardial infarction. Oncotype DX, a gene expression panel, helps guide adjuvant therapy in breast cancer. Molecular signatures such as FLT3 mutations in leukemia dictate specific targeted therapies.
The future lies in expanding this biomarker universe through multi-omics—integrating genomics, proteomics, metabolomics, and beyond. Such data-rich approaches align perfectly with RTR, offering not only mechanistic insights but also the foundation for truly personalized medicine.
Precision Medicine and the Promise of Personalization
Precision medicine is not merely a fashionable phrase; it is the logical extension of reverse translation. By accounting for genetic, molecular, and environmental differences among patients, precision medicine moves away from “one-size-fits-all” therapy.
RTR feeds this paradigm. By studying real patients and tracing their variable responses back to molecular drivers, researchers can identify predictive biomarkers and stratify patients accordingly. Instead of discarding non-responders as statistical noise, RTR seeks to understand them.
The clinical implications are profound:
- Reduced trial-and-error prescribing.
- Minimized adverse effects by avoiding futile therapies.
- Enhanced efficiency in clinical trials through patient stratification.
The irony is not lost: medicine is finally embracing what every physician has known intuitively for centuries—patients are individuals, not averages. Precision medicine, powered by reverse translation, allows science to honor that reality.
Rapid Translation in Crises: Lessons from COVID-19
The COVID-19 pandemic showcased RTR in real time. Faced with a novel virus and no established therapies, clinicians observed, experimented, and repurposed. Drugs such as remdesivir, dexamethasone, and baricitinib entered clinical practice at record speed, guided by a mixture of bedside observation and mechanistic follow-up.
Though not all efforts succeeded (remember hydroxychloroquine?), the process demonstrated the agility of RTR. Rather than waiting for years of preclinical refinement, scientists and physicians collaborated in iterative cycles: clinical data informed laboratory studies, which in turn refined ongoing trials.
The urgency of the pandemic accelerated acceptance of RTR as not just an academic curiosity but a practical necessity in global health emergencies. One hopes the lesson is not forgotten as the world confronts other pressing crises, from antimicrobial resistance to neurodegenerative diseases.
Challenges and Limitations
No paradigm is without hurdles, and RTR is no exception. Its challenges are formidable:
- Data complexity: Patient-derived data are messy, heterogeneous, and often incomplete.
- Modeling difficulties: Translating bedside observations into mechanistic models requires creativity and rigor.
- Ethical concerns: Use of patient data raises questions of consent, privacy, and equitable benefit sharing.
- Infrastructure needs: RTR demands robust biobanking, advanced analytics, and interdisciplinary collaboration.
Moreover, the cultural inertia of science is real. Laboratories are accustomed to hypothesis-driven, controlled experiments. Clinicians are trained to treat, not to generate mechanistic hypotheses. Bridging these worlds requires new training, incentives, and institutional support.
Yet, none of these obstacles are insurmountable. Indeed, they reflect the growing pains of a paradigm still finding its footing.
The Future of Reverse Translational Research
Where might RTR lead us? The prospects are tantalizing. As omics technologies expand, as artificial intelligence refines data mining, and as global data-sharing initiatives mature, the power of RTR will only grow.
Imagine a future in which every patient encounter generates digital data—genomic, biochemical, physiological—that feeds into a global research network. Unusual responses are flagged, mechanisms investigated, therapies refined, and results disseminated in real time. The loop between bedside and bench becomes shorter, tighter, and more productive.
This is not science fiction; it is the logical trajectory of modern biomedicine. Reverse translational research, by honoring the patient as the ultimate teacher, could finally align drug discovery with the messy, beautiful reality of human biology.
Conclusion
Drug discovery is at a crossroads. The traditional bench-to-bedside highway, though valuable, has reached its limits. Reverse translational research offers a complementary route: begin with patients, learn from them, and let their stories guide science.
It is a paradigm that prizes relevance over elegance, humility over hubris, and pragmatism over perfection. By embracing RTR, medicine may not only accelerate discovery but also restore its central focus: the patient. After all, what greater laboratory could there be than the lived experience of human health and disease?
FAQ
1. How does reverse translational research differ from traditional translational research?
Traditional translational research moves from laboratory discovery to clinical application. Reverse translational research inverts the process—starting with patient observations and feeding them back into basic science for mechanistic exploration.
2. Why is reverse translational research important for drug discovery?
Because most drugs fail in late-phase trials, largely due to poor predictive power of preclinical models. RTR grounds research in real patient outcomes, improving relevance, efficiency, and the likelihood of clinical success.
3. What are some real-world examples of reverse translational research?
Drug repurposing provides clear examples: sildenafil for erectile dysfunction, minoxidil for hair growth, thalidomide for multiple myeloma, and remdesivir for COVID-19. Each began with clinical observations that redirected research and ultimately created new therapies.