Introduction
Erectile dysfunction (ED) is often regarded as a disease of aging, yet an increasing body of evidence has disrupted this stereotype. Alarmingly, a growing number of young men under 40 years are presenting with ED. For a sizable proportion of them, the etiology is not vascular or endocrine but psychological. This condition, termed non-organic erectile dysfunction (NOED), is now a major clinical challenge.
In Pakistan, recent surveys have revealed that more than half of men under 40 with ED demonstrate a psychogenic origin. These young men may carry intact hormonal and vascular systems, yet they are trapped in cycles of anxiety, maladaptive cognition, and relationship stress that undermine sexual function. For clinicians, this has profound implications: prescribing a phosphodiesterase-5 inhibitor (PDE5I) alone may provide transient relief, but for many, the root of dysfunction lies beyond pharmacology.
The randomized placebo-controlled trial conducted by Bilal and Abbasi (2022) explored this dilemma. By comparing sildenafil citrate (SC), cognitive behavior sex therapy (CBST), integrated treatment, and placebo, the study offered a rare, data-driven perspective on what actually works for NOED. This article unpacks their findings, explores the psychosexual underpinnings of NOED, and argues for a more integrative model of care.
Non-Organic Erectile Dysfunction: Understanding the Problem
NOED is not about defective arteries or low testosterone; it is about the mind’s interference with the body’s natural capacity for arousal. Patients often present with persistent difficulty achieving or maintaining erections despite normal vascular and hormonal evaluations. This paradox frustrates both patients and clinicians, as the absence of clear biomarkers makes NOED a diagnosis of exclusion.
Psychological triggers are varied. Anxiety—particularly performance anxiety—is the most common culprit. Once a man experiences a failed erection, the memory itself becomes a source of anticipatory fear, further fueling dysfunction. Depression also plays a role, blunting desire and impairing arousal. Relationship discord, lack of sexual education, and maladaptive beliefs about masculinity or intimacy compound the problem.
Young men are particularly vulnerable. Studies from Pakistan highlight that in men under 40, psychogenic causes outnumber organic ones by more than two to one. Cultural factors further complicate matters: limited access to sexual education, stigma around discussing intimacy, and high expectations regarding sexual performance make NOED a potent source of distress.
For decades, treatment protocols focused almost exclusively on PDE5Is like sildenafil. These drugs amplify nitric oxide–mediated vasodilation, producing erections in response to stimulation. Yet, their effect is mechanical, not psychological. In NOED, PDE5Is often fail to restore satisfaction because they do not address anxiety, maladaptive thoughts, or relational issues. This is where psychotherapy enters the equation.
Cognitive Behavior Sex Therapy: A Modern Psychosexual Tool
CBST is an adaptation of cognitive-behavioral therapy (CBT) designed specifically for sexual dysfunction. It merges traditional sex therapy—focused on education, communication, and behavioral exercises—with cognitive restructuring techniques.
At its core, CBST challenges the automatic negative thoughts that plague men with NOED. Patients learn to identify self-defeating beliefs (“I will fail again,” “I am not masculine enough”), reframe them through Socratic questioning, and replace them with healthier cognitions. Alongside, behavioral assignments such as the “stop–start technique,” mindfulness exercises, and structured intimacy tasks reduce performance anxiety and reintroduce sexual pleasure without pressure.
The therapy is not limited to the clinic. Homework assignments encourage men to practice communication with partners, experiment with non-penetrative intimacy, and build confidence gradually. Over time, these exercises dismantle the psychological barriers that pills cannot touch.
Evidence has shown that CBST alone can significantly improve erectile function in NOED. It enhances not only erection quality but also satisfaction with intercourse, reduction in anxiety, and overall sexual confidence. Still, for many men, a purely psychological approach may take time to deliver visible results, and dropout rates remain a concern. This is where integration with pharmacotherapy proves transformative.
The Mosul Study Revisited: Methodology in Focus
Bilal and Abbasi conducted a 12-week randomized placebo-controlled trial in South Punjab, Pakistan. A total of 137 men aged 18–39 years with NOED were recruited; 116 completed the study. They were randomized into four groups:
- Sildenafil citrate (SC) group – On-demand 50 mg SC, one hour before intercourse.
- CBST group – Twice-weekly 50-minute sessions, supplemented by homework assignments.
- Integrated treatment group – Combination of SC and CBST.
- Placebo group – Placebo tablets taken under the same protocol as SC.
Outcomes were measured using the International Index of Erectile Function-5 (IIEF-5) and the Depression Anxiety Stress Scale-21 (DASS-21). Assessments were performed pre-treatment, post-treatment, and 12 weeks after treatment completion.
This design allowed a robust comparison not only of efficacy in improving erectile function but also of secondary outcomes—namely depression and anxiety reduction. The use of validated Urdu translations of both tools ensured cultural appropriateness.
Key Findings: More Than Just Erections
The results of the trial were illuminating.
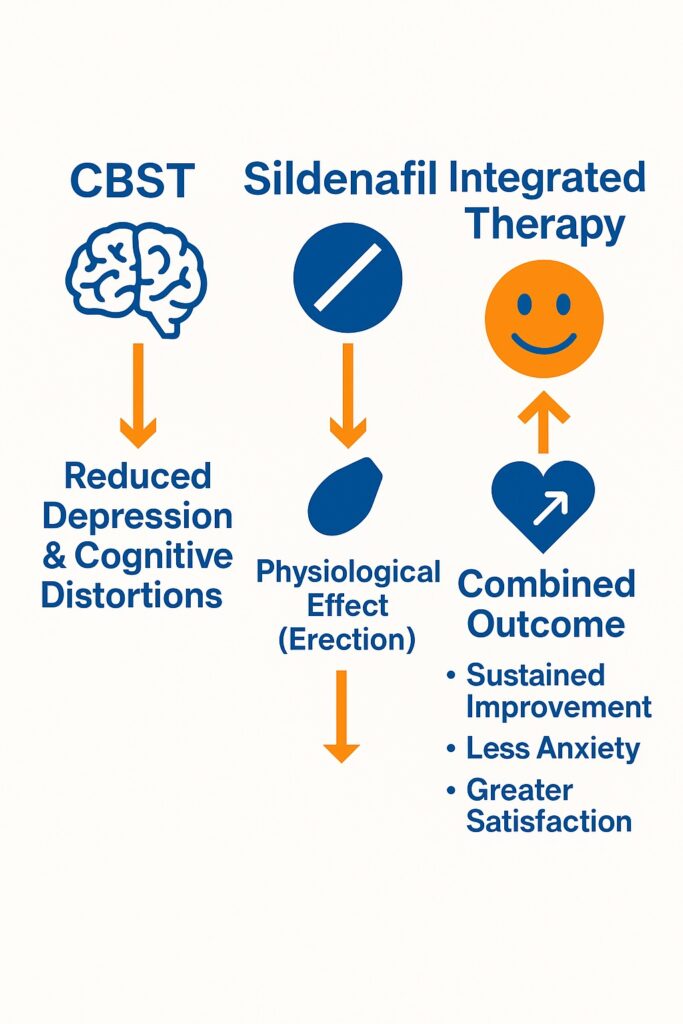
First, both CBST and integrated treatment groups demonstrated significant improvement in IIEF-5 scores compared to placebo. In other words, psychotherapy was just as effective as pharmacotherapy, if not more so, in addressing NOED. Interestingly, the integrated group showed marginally higher improvements in erectile function than either treatment alone, though the difference was not dramatic.
Second, CBST excelled in reducing depression. Participants in this group showed greater alleviation of depressive symptoms compared to those who received SC or integrated therapy. This suggests that by directly targeting maladaptive cognitions, CBST improves not just sexual function but also broader psychological well-being.
Third, the integrated treatment was uniquely effective in reducing anxiety. By pairing the immediate physiological aid of sildenafil with the long-term restructuring of CBST, the integrated approach provided dual relief—erections became easier to achieve, and the psychological burden of performance anxiety was lifted.
Fourth, neither age nor duration of NOED significantly influenced treatment outcomes. This finding emphasizes that therapy should not be delayed or stratified solely on these parameters; psychological interventions are valuable regardless of patient age or symptom chronicity.
Clinical Implications: Toward a New Standard of Care
The implications of this study are profound. For decades, men with ED have been treated almost reflexively with PDE5Is. While these drugs revolutionized management, they are far from a panacea—particularly for NOED. The evidence now points toward integrated care as the true gold standard.
CBST, either alone or in combination with sildenafil, directly addresses the psychogenic roots of dysfunction. It restores not only erections but also confidence, intimacy, and mental health. In cultures where stigma around sexual failure is high, this holistic approach is invaluable.
Clinicians should therefore consider several practical steps:
- Screen for psychological contributors – Depression, anxiety, maladaptive beliefs, and relational stress must be assessed alongside vascular and hormonal factors.
- Offer psychotherapy as first-line – For young men with clear psychogenic ED, CBST should be prioritized, either alone or combined with pharmacotherapy.
- Use integrated therapy for resistant cases – Men who fail PDE5Is or remain anxious despite therapy may benefit most from integration.
By shifting focus from symptom control to root-cause resolution, integrated therapy can transform outcomes for young men struggling with NOED.
Challenges and Limitations
While promising, the trial was not without limitations. First, medical evaluations to conclusively exclude organic ED were limited; subtle vascular or endocrine factors may have been overlooked. Second, recruitment relied on purposive and snowball sampling, introducing potential bias. Third, blinding was imperfect, particularly in the CBST group, where participants were aware of their treatment allocation.
Moreover, only sildenafil was tested among PDE5Is. Agents like tadalafil, with longer half-lives, might interact differently with psychotherapy. Finally, outcome measures focused on erectile function and psychological distress, but did not capture relational satisfaction or partner perspectives—important domains in real-world sexual health.
These limitations highlight the need for larger, multicenter trials with broader endpoints. Still, the consistency of findings across Pakistani and international studies lends credibility to the integrated approach.
Broader Reflections: Why Integration Matters
The success of integrated therapy reflects a broader truth in medicine: complex conditions rarely yield to single interventions. Just as diabetes requires both insulin and lifestyle change, NOED demands both pharmacological support and psychological restructuring.
Sildenafil may break the cycle of failure by guaranteeing an erection. But without dismantling the anxious thoughts and faulty beliefs that triggered NOED, the problem will resurface as soon as the pill is withdrawn. Conversely, CBST may eventually rebuild confidence, but progress is slow, and early dropout is a risk if men do not experience tangible improvements quickly.
Together, the two approaches cover each other’s weaknesses. Sildenafil provides the immediate reassurance of performance, while CBST ensures durable psychological change. The combination is greater than the sum of its parts—a principle that should guide modern sexual medicine.
Conclusion
Non-organic erectile dysfunction is an increasingly common challenge in young men worldwide. It arises not from diseased vessels or hormones but from psychological and relational disturbances. As the study by Bilal and Abbasi demonstrated, effective treatment requires more than pills.
CBST and integrated therapy both significantly improve erectile function, reduce psychological distress, and offer durable benefits. While sildenafil alone may offer short-term relief, it fails to address the deeper anxieties and depressive symptoms that perpetuate dysfunction.
The future of NOED management lies in integration—melding the precision of pharmacology with the depth of psychotherapy. By adopting such holistic strategies, clinicians can not only restore erections but also heal relationships, rebuild confidence, and enhance overall mental health.
FAQ
1. Can sildenafil alone cure non-organic erectile dysfunction?
Not entirely. While sildenafil can produce erections, it often fails to resolve the underlying psychological causes of NOED. Many men relapse once the drug is stopped.
2. How does CBST differ from standard psychotherapy?
CBST specifically targets sexual beliefs, performance anxiety, and relational dynamics. It combines cognitive restructuring with behavioral techniques such as mindfulness and communication training, making it tailored for sexual dysfunction.
3. What is the advantage of integrated treatment?
Integrated therapy combines the rapid physiological effect of sildenafil with the durable psychological restructuring of CBST. This dual approach improves erectile function, reduces anxiety, and enhances satisfaction more effectively than either treatment alone.


