Introduction
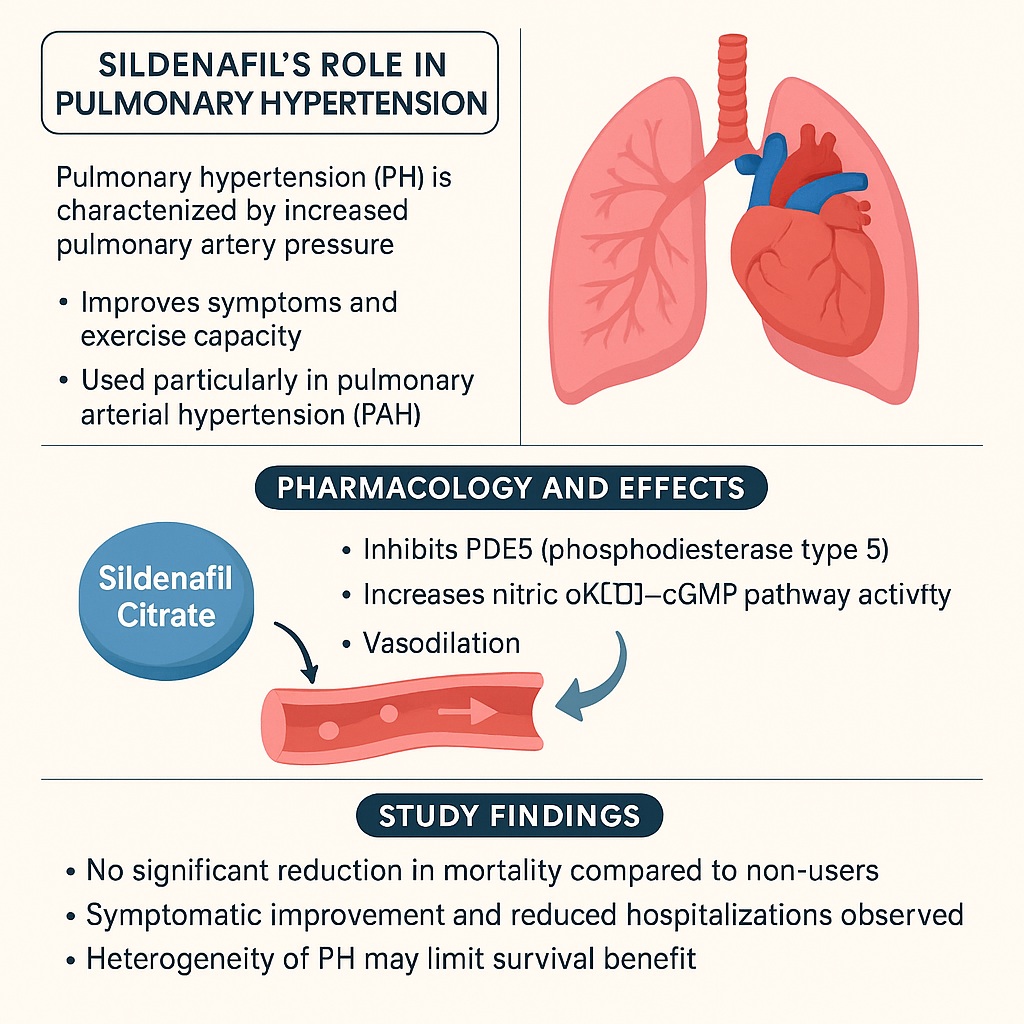
Sildenafil citrate has traveled a fascinating journey since its discovery. Originally synthesized as a potential anti-anginal agent, it famously redefined itself as Viagra, a breakthrough treatment for erectile dysfunction. Later, the same pharmacological properties that improved penile blood flow were harnessed for another purpose: pulmonary arterial hypertension (PAH). By selectively inhibiting phosphodiesterase type 5 (PDE5), sildenafil enhances nitric oxide–mediated vasodilation and reduces pulmonary vascular resistance. This made it one of the few effective oral therapies for PAH, a progressive, life-limiting disease characterized by increased pulmonary artery pressure and right ventricular dysfunction.
Yet, despite its therapeutic promise, questions remain. Sildenafil is generally well tolerated, but its long-term impact on survival in patients with pulmonary hypertension is still debated. Clinical trials, often limited in size and duration, offer valuable insights but may not reflect the full complexity of real-world practice. The study underlying this discussion aimed to address precisely that gap—examining mortality risk among sildenafil users in a large, real-world population of patients with pulmonary hypertension.
This article explores the pharmacological basis of sildenafil in PAH, evaluates the clinical design and findings of the recent study, and discusses broader implications for medical practice. Along the way, it sheds light on how data drawn from daily clinical reality sometimes complicate the neat conclusions of controlled trials.
The Rationale for Sildenafil in Pulmonary Hypertension
Pulmonary hypertension represents a spectrum of conditions defined by elevated pulmonary arterial pressures and secondary right ventricular strain. Among its subgroups, pulmonary arterial hypertension is the best characterized, though pulmonary hypertension may also arise secondary to left heart disease, lung disease, or chronic thromboembolic events. Regardless of origin, the condition ultimately converges on a vicious cycle of increased pulmonary resistance, right ventricular overload, and progressive right heart failure.
The molecular rationale for sildenafil’s use lies in the nitric oxide–cGMP pathway. In healthy individuals, nitric oxide stimulates guanylyl cyclase, increasing cGMP levels and promoting vasodilation. PDE5 rapidly degrades cGMP, limiting the extent of vasodilation. By blocking PDE5, sildenafil prolongs cGMP activity, reduces vascular tone, and improves hemodynamic efficiency. Unlike calcium channel blockers, which only help a minority of PAH patients responsive to vasoreactivity testing, sildenafil acts broadly on pulmonary vascular remodeling and has become a mainstay of therapy.
Previous randomized controlled trials demonstrated sildenafil’s ability to improve exercise capacity, symptoms, and pulmonary hemodynamics. However, survival benefit has been less consistently proven. While surrogate endpoints such as 6-minute walk distance or cardiac index may improve, whether these translate into reduced mortality has remained an open question.
Study Design and Methodological Considerations
The real-world study in question leveraged a national health database to identify patients diagnosed with pulmonary hypertension who were treated with sildenafil. It compared outcomes—primarily mortality risk—between sildenafil users and matched non-users. This retrospective cohort design allowed inclusion of thousands of patients, a scale unattainable for most randomized controlled trials in this rare disease.
Patients were included if they had a confirmed diagnosis of pulmonary hypertension, defined according to contemporary hemodynamic criteria. Exclusions applied to those with incomplete records, advanced comorbidities, or concomitant use of investigational therapies. Exposure to sildenafil was defined as documented prescription records, with treatment duration and adherence verified through pharmacy refill data. Controls were matched based on demographics, comorbidities, and disease severity indicators.
Mortality was assessed as the primary endpoint, with additional analyses on hospitalization, disease progression, and adverse events. Statistical methods included Cox proportional hazards models and sensitivity analyses to minimize confounding.
By design, such studies cannot achieve the rigor of a blinded randomized trial. However, they offer a broader lens, capturing variations in practice patterns, comorbidity burden, and adherence—all of which influence real-world outcomes.
Key Findings: Sildenafil and Mortality Risk
The study yielded nuanced results. On one hand, sildenafil use was associated with symptomatic improvement and reduced hospitalizations, aligning with earlier controlled trial findings. Patients reported improved exercise tolerance, and markers of right heart strain were attenuated. On the other hand, the central question—did sildenafil reduce mortality?—was more complex.
Overall, mortality among sildenafil users was not significantly lower than in matched non-users. In certain subgroups, such as patients with idiopathic PAH, modest trends toward survival benefit were noted, but statistical significance was lacking. Conversely, in patients with pulmonary hypertension secondary to left heart disease, sildenafil offered no mortality benefit and in some cases was associated with worse outcomes, possibly due to systemic hypotension or fluid retention.
These findings highlight the heterogeneity of pulmonary hypertension. A therapy effective in one subgroup may not translate across the spectrum, and assumptions of universal benefit can be misleading. For clinicians, the results emphasize tailoring therapy not only to disease category but also to the individual patient’s risk profile.
Mechanistic Interpretations: Why Mortality Impact May Be Limited
Why might sildenafil improve symptoms and hemodynamics without significantly altering survival? Several possibilities exist.
First, sildenafil’s mechanism is largely vasodilatory and symptomatic. While it alleviates pressure overload and improves exercise tolerance, it may not fundamentally reverse pulmonary vascular remodeling, which is the true driver of long-term prognosis in PAH. Structural changes in pulmonary arteries—including intimal fibrosis and smooth muscle hypertrophy—remain largely unaffected.
Second, disease heterogeneity dilutes outcomes. PAH is distinct from pulmonary hypertension caused by left heart disease or lung disease. In the latter, sildenafil may improve pulmonary circulation but exacerbate systemic hemodynamics, blunting its net effect on survival.
Third, real-world adherence may differ from trial conditions. Missed doses, drug–drug interactions, and suboptimal titration may reduce effectiveness. Moreover, comorbidities common in older PH populations—hypertension, diabetes, chronic kidney disease—may overshadow the modest benefits of sildenafil.
Thus, while sildenafil clearly addresses part of the problem, its impact on the natural history of pulmonary hypertension may remain modest, unless combined with other targeted therapies.
Clinical Implications: Applying Evidence to Practice
For clinicians, the take-home message is not to abandon sildenafil, but to use it wisely. It remains a valuable therapy, particularly in idiopathic or heritable PAH, where symptom relief and improved functional status are meaningful. However, prescribing sildenafil indiscriminately to all forms of pulmonary hypertension may lead to disappointment—or harm.
Patients with PH secondary to left heart failure or chronic lung disease should not be assumed to benefit. In fact, guideline bodies now caution against PDE5 inhibitors in these populations outside of clinical trials. For idiopathic PAH, sildenafil remains a first-line oral option, often combined with endothelin receptor antagonists or prostacyclin analogues in dual or triple therapy regimens. The study reinforces the importance of multidisciplinary care, frequent reassessment, and escalation when monotherapy fails.
Additionally, the lack of clear survival benefit should temper expectations. Patients must be counseled honestly: sildenafil will likely help them feel better and function better, but whether it prolongs life remains uncertain. Transparency fosters adherence and trust.
The Broader Context: Real-World Data vs. Clinical Trials
This study also underscores a broader tension in modern medicine: the divergence between randomized controlled trials and real-world evidence. Controlled trials are indispensable for establishing efficacy, but they often exclude patients with comorbidities, advanced age, or polypharmacy. Real-world studies, while less rigorous, reflect the messy reality of clinical practice. Reconciling these perspectives is essential for evidence-based medicine.
In the case of sildenafil for pulmonary hypertension, both views matter. Randomized trials confirm its biological plausibility and symptomatic benefit. Real-world data, however, remind us that survival outcomes may not always follow. Together, they encourage nuanced prescribing and highlight the need for ongoing surveillance of drug effectiveness beyond regulatory approval.
Conclusion
Sildenafil citrate remains a cornerstone therapy in the management of pulmonary arterial hypertension, offering symptomatic relief and functional improvement. Yet, its effect on long-term survival appears limited, particularly when used outside the idiopathic PAH subgroup. Real-world evidence complements trial data by illuminating these limitations, reminding clinicians of the heterogeneity of pulmonary hypertension and the need for tailored therapy.
Rather than a panacea, sildenafil should be viewed as one instrument in a broader therapeutic symphony. Its value lies in improving quality of life and bridging patients to more advanced therapies. The ultimate goal—extending survival—will likely require multimodal strategies that address not only vasodilation but also vascular remodeling and right ventricular adaptation.
FAQ
1. Does sildenafil improve survival in pulmonary hypertension?
Not conclusively. While it improves symptoms and exercise tolerance, real-world studies suggest that its effect on mortality is limited, except perhaps in idiopathic PAH.
2. Should sildenafil be prescribed for all types of pulmonary hypertension?
No. Its benefits are mainly established in pulmonary arterial hypertension. In PH secondary to left heart disease or lung disease, sildenafil may be ineffective or even harmful.
3. What should patients expect when starting sildenafil for PAH?
Most patients can expect improved breathing, exercise tolerance, and quality of life. However, survival benefit is uncertain, and ongoing monitoring is crucial to assess whether therapy should be continued or combined with other agents.


