Introduction
Sildenafil citrate, more popularly recognized under its brand name Viagra, is celebrated as a revolutionary treatment for erectile dysfunction. Since its approval by the U.S. Food and Drug Administration in 1998, it has been widely used by millions of men worldwide. Later, its clinical application expanded to pulmonary arterial hypertension and benign prostatic hyperplasia, supported by its pharmacological profile as a phosphodiesterase-5 (PDE5) inhibitor. By augmenting nitric oxide–mediated vasodilation, sildenafil improves smooth muscle relaxation and blood flow in multiple tissues. Its therapeutic reach now extends into explorations of diabetes and chronic kidney disease management. However, the “blue pill” also carries risks that are less widely acknowledged, especially in ophthalmology.
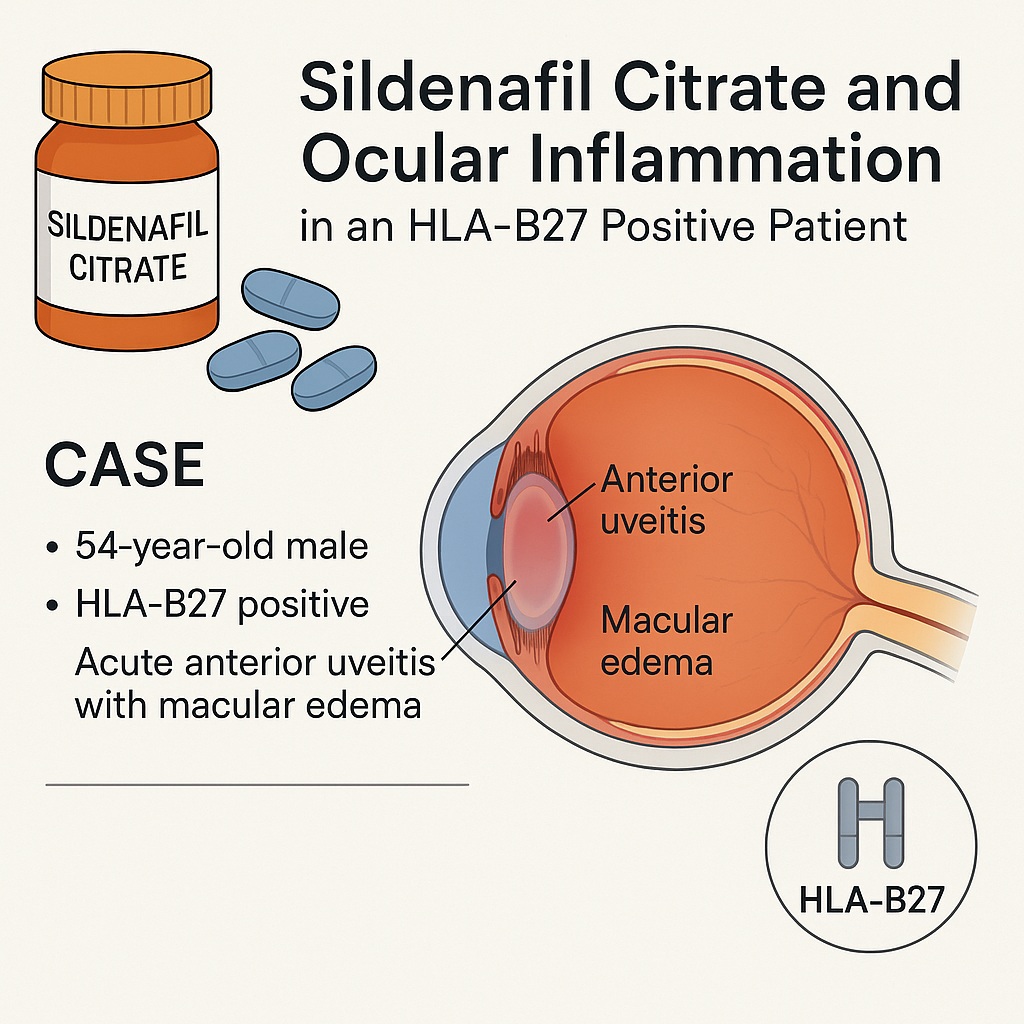
While transient disturbances in color vision, brightness perception, and subtle changes in electroretinography have long been recognized, there is increasing concern regarding more serious ocular complications. Among these, non-arteritic anterior ischemic optic neuropathy, serous macular detachments, and even intraocular hemorrhages have been reported. The case described in the literature highlights something more unusual: the onset of acute anterior uveitis with macular edema after sildenafil use in a patient carrying the HLA-B27 genetic marker. This single patient case offers valuable insight into how genetic predisposition and pharmacological triggers may interact in unexpected ways.
Case Overview: When Sildenafil Meets Predisposition
The subject was a 54-year-old Caucasian male with no significant ocular or systemic disease history. His only prior ophthalmic procedure was bilateral LASIK over a decade earlier. Following his very first dose of sildenafil, he developed redness, irritation, and photophobia in the left eye. Clinical examination confirmed acute anterior uveitis (AAU), with slit-lamp findings of ciliary injection, keratic precipitates, and mild anterior chamber inflammation. Importantly, spectral-domain optical coherence tomography (SD-OCT) identified parafoveal hyperreflective subretinal deposits.
Initial treatment with topical corticosteroids brought symptomatic relief. However, upon a second trial of sildenafil, symptoms returned with increased severity. This time, vision decreased to 20/40, and imaging revealed cystoid macular edema. Fluorescein angiography showed macular leakage in both eyes, though edema was limited to the left. Blood work identified HLA-B27 positivity, while all other systemic investigations—including syphilis, tuberculosis, sarcoidosis, and Behçet’s disease—were negative.
After discontinuation of sildenafil and continuation of topical steroids, the patient’s inflammation resolved, and vision improved to baseline within three months. No further recurrences occurred once sildenafil was avoided, underscoring its likely role as the precipitating factor.
HLA-B27 and Ocular Vulnerability
Anterior uveitis is the most common type of uveitis, representing up to 90% of cases in primary care and more than half in tertiary ophthalmic centers in Western countries. Among its etiologies, HLA-B27 positivity plays a pivotal role. Around 50% of patients with recurrent unilateral anterior uveitis carry this allele, and many also develop systemic diseases such as ankylosing spondylitis. In fact, nearly 90% of individuals with ankylosing spondylitis are HLA-B27 positive, and roughly 40% will experience acute anterior uveitis at some point.
This genetic predisposition creates a fertile ground for inflammatory events. In this case, sildenafil appears to have acted as the spark. The genetic background provided the susceptibility; the pharmacological agent provided the trigger. The intersection of these two risk factors offers a reminder that even drugs considered relatively safe can act unpredictably in genetically predisposed individuals.
Sildenafil’s Ocular Effects Beyond Color Vision
The visual system is not a primary target of PDE5 inhibitors, yet the drug does not leave it untouched. Sildenafil is known to partially inhibit phosphodiesterase-6 (PDE6), which is localized in retinal photoreceptors. This “off-target” effect explains why users often report transient changes in color discrimination and brightness perception. Fortunately, these effects are usually reversible and benign.
More concerning are the reports linking sildenafil to vision-threatening complications. Documented associations include:
- Anterior ischemic optic neuropathy, leading to sudden, irreversible vision loss.
- Serous macular detachments, which disrupt retinal architecture and impair vision.
- Intraocular hemorrhages and hyphema, particularly in patients with diabetic retinopathy.
Such cases prompted the FDA to issue warnings, advising patients to discontinue PDE5 inhibitors and seek urgent medical care if sudden vision changes occur. Against this backdrop, the case of sildenafil-associated anterior uveitis with macular edema adds yet another layer of complexity.
Mechanistic Hypotheses: How Could Sildenafil Trigger Uveitis?
Understanding the pathophysiology behind this adverse reaction requires a synthesis of pharmacology and immunogenetics. Several hypotheses emerge:
- Vascular Effects
Sildenafil increases choroidal blood flow by relaxing smooth muscle in choroidal vessels, akin to its effect on penile vasculature. This increase in ocular perfusion could, in theory, exacerbate or reveal subclinical inflammation, ultimately leading to macular edema. - Immune Modulation
Interestingly, sildenafil has demonstrated anti-inflammatory properties in animal models and some human studies. However, paradoxical effects are possible, particularly in predisposed individuals. In the HLA-B27 positive patient, sildenafil may have tipped the balance toward overt inflammation. - Drug-Induced Uveitis Mechanisms
Uveitis secondary to medication can occur via direct toxicity to ocular tissues or indirectly through immune-mediated pathways. In this case, the latter seems more plausible, as sildenafil has otherwise been linked to reduced inflammation in other contexts. Its role may lie in augmenting vascular permeability or destabilizing an already fragile blood-ocular barrier.
While these mechanisms remain speculative, the temporal relationship between sildenafil intake and uveitis onset, combined with the reproducibility of symptoms upon rechallenge, strengthens the case for causality.
Lessons from the Literature: Similar Stories, Different Contexts
This report is not entirely without precedent. A similar case described recurrent posterior uveitis in a patient with Behçet’s disease who had remained ophthalmologically quiet for over a decade—until sildenafil was introduced. Likewise, other ocular adverse events have been observed across various conditions, suggesting that sildenafil’s impact is magnified in patients with underlying vulnerabilities.
Drug-induced uveitis is not unique to PDE5 inhibitors. A wide range of agents—including bisphosphonates, tumor necrosis factor-α inhibitors, sulfonamides, and cidofovir—are known culprits. The challenge lies in distinguishing coincidence from causation, particularly in conditions like uveitis, where idiopathic cases remain common.
Clinical Implications and Practical Guidance
For the practicing ophthalmologist or physician, this case offers several important reminders:
- Genetic predisposition matters. Patients with HLA-B27 positivity or other autoimmune risk factors may react differently to medications considered benign in the general population.
- Medication history is essential. Even seemingly unrelated drugs like sildenafil should be included in a thorough review, particularly in first-time uveitis presentations.
- Discontinuation and monitoring work. Once the offending drug is withdrawn, inflammation often resolves, as was evident in this case.
From a patient counseling perspective, the advice is straightforward: if new ocular symptoms arise after initiating sildenafil or other PDE5 inhibitors, immediate evaluation is warranted. Clinicians should resist dismissing such complaints as trivial, given the potential for sight-threatening complications.
A Glimpse Ahead: The Research Needed
The rarity of this adverse reaction means large-scale studies are unlikely to provide definitive answers soon. Nevertheless, case reports remain valuable as early warning signals. Collaborative registries of ocular drug reactions could help identify patterns and clarify mechanisms. Additionally, genetic screening may one day guide safer prescribing practices, flagging those at risk for unexpected drug-induced complications.
For now, prudence dictates caution. The combination of HLA-B27 positivity and sildenafil use may represent a niche but real risk for ocular inflammation, meriting further exploration by ophthalmology and pharmacology communities alike.
Conclusion
Sildenafil citrate remains a highly effective and generally safe therapy for erectile dysfunction and other vascular conditions. Yet, as this case underscores, even well-established drugs can provoke rare and unexpected complications in predisposed individuals. The onset of acute anterior uveitis with macular edema in an HLA-B27 positive patient illustrates how pharmacological action and genetic susceptibility can intersect with clinical significance. While further studies are needed, physicians should remain vigilant, ensuring that patients at higher risk are adequately counseled and monitored.
FAQ
1. Can sildenafil really cause uveitis, or was this just coincidence?
The temporal association, recurrence upon rechallenge, and resolution after discontinuation strongly suggest a causal link in this case. While rare, drug-induced uveitis is a recognized phenomenon, and sildenafil appears capable of triggering it in genetically predisposed individuals.
2. Should all patients with HLA-B27 positivity avoid sildenafil?
Not necessarily. The vast majority tolerate the drug without issue. However, patients with a history of uveitis or known HLA-B27–related disease should use sildenafil cautiously, and any new ocular symptoms should prompt immediate medical review.
3. What symptoms should raise concern after taking sildenafil?
Redness, photophobia, blurred vision, or sudden changes in visual acuity should not be ignored. These may indicate anterior uveitis, macular edema, or other ocular complications. Prompt ophthalmologic evaluation is essential to prevent lasting damage.


